Published on March 17, 2021
Individuals hospitalized for cardiovascular and cerebrovascular events were more likely to have poor outcomes if vitamin D deficient
 According to the World Health Organization, close to 18 million people worldwide die each year from cardiovascular diseases (31% of all deaths) and 85% of those deaths are due to heart attacks and strokes. Previously, GrassrootsHealth has covered the correlation between cardiovascular diseases and the status of different nutrients, such as vitamin D, omega-3s, and magnesium. Vitamin D in particular has been associated with lower blood pressure, reduced risk of arterial stiffness, diabetes and insulin resistance, as well as maintaining glucose regulation and a healthy lipid profile.
According to the World Health Organization, close to 18 million people worldwide die each year from cardiovascular diseases (31% of all deaths) and 85% of those deaths are due to heart attacks and strokes. Previously, GrassrootsHealth has covered the correlation between cardiovascular diseases and the status of different nutrients, such as vitamin D, omega-3s, and magnesium. Vitamin D in particular has been associated with lower blood pressure, reduced risk of arterial stiffness, diabetes and insulin resistance, as well as maintaining glucose regulation and a healthy lipid profile.
Vitamin D also plays an important role in brain health and could help prevent strokes and other cerebrovascular disease, as well as benefit those who’ve already had a stroke. Vitamin D supports normal neuron function and prevents cellular death after a brain injury. Studies, such as the one reviewed below, have linked low vitamin D levels with increased stroke severity and a higher risk of post-stroke disability and mortality.
Could Vitamin D Levels Affect the Prevalence and Severity of Cardiovascular and Cerebrovascular Disease Events?
Patel et al. performed a cross-sectional study of adult patients who had been hospitalized for cardiovascular disease (angina, myocardial infarction, arrhythmia, and congestive heart failure) and/or cerebrovascular disorders (acute ischemic stroke, transient ischemic attack, intracerebral hemorrhage and subarachnoid hemorrhage), who were also diagnosed with vitamin D deficiency at the time of hospitalization. (Note that vitamin D deficiency was determined based on a reported diagnosis code (ICD-10), not on a specified lab value.)
The aim of the study was to determine the prevalence of these disorders among those with vitamin D deficiency in comparison with those not diagnosed with vitamin D deficiency, and to find out if those with vitamin D deficiency experienced worse outcomes (such as severe or extreme loss of function and disability) or were more likely to be discharged to a non-home facility after hospitalization. Independent variables were also identified and accounted for, including comorbidities of hypertension, diabetes, obesity, hypercholesterolemia, smoker, and renal dysfunction.
What did the study find?
1,059,755 patients were identified with vitamin D deficiency. Among patients admitted with different cardiovascular (CVD) and cerebrovascular (CeVD) conditions, the prevalence of congestive heart failure, acute ischemic stroke, and transient ischemic attack was significantly higher among those with vitamin D deficiency compared to those without deficiency. The study also found that those with vitamin D deficiency had significantly higher rates of severe or extreme disability following the events, and non-home discharge from the hospital, compared to those without.
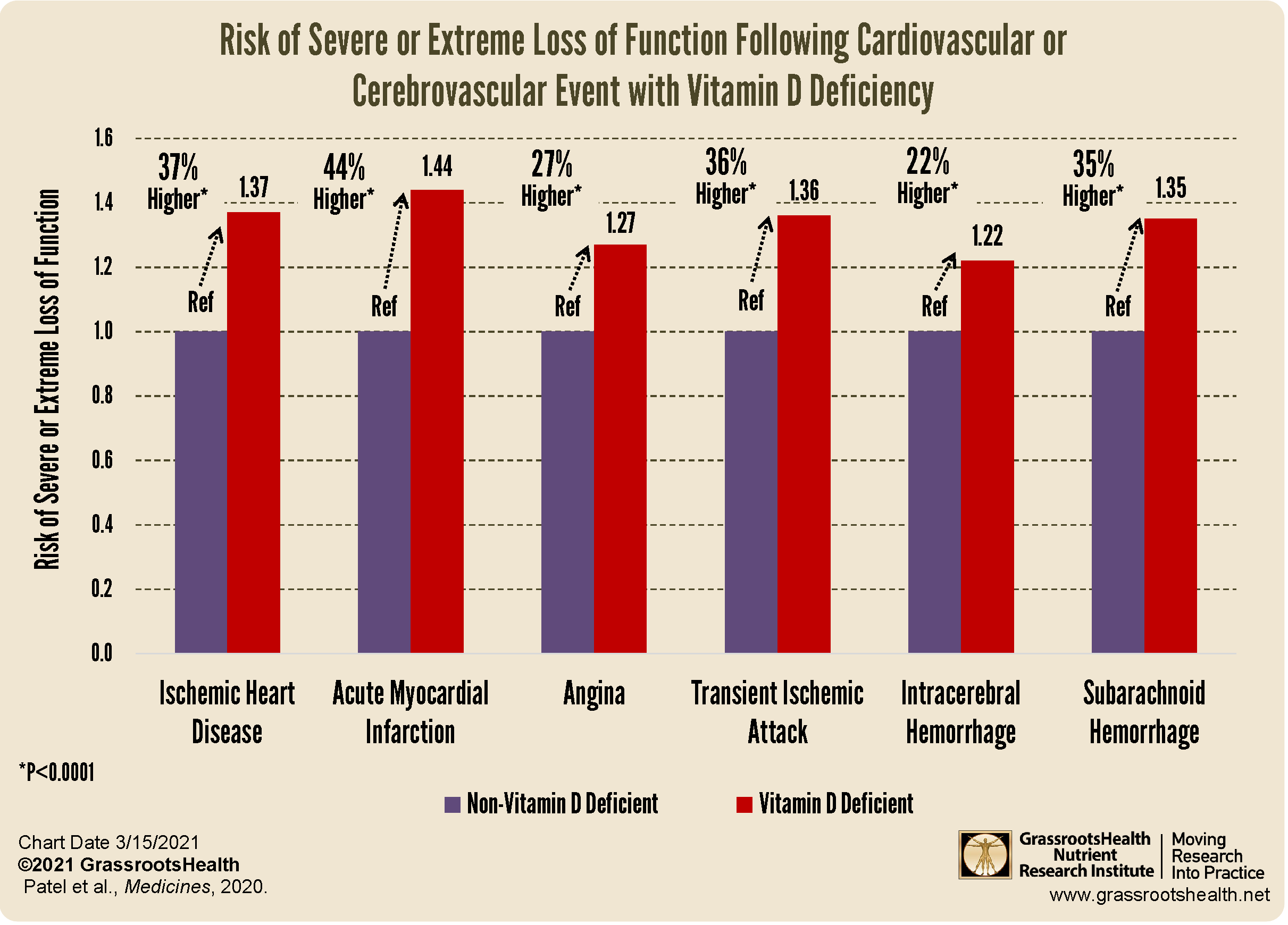
As illustrated in the chart above, the risk of severe or extreme loss of function was greater among those with a diagnosis of vitamin D deficiency compared to those without vitamin D deficiency (p<0.0001), specifically:
- 37% higher for Ischemic Heart Disease
- 44% higher for Acute Myocardial Infarction (Heart Attack)
- 27% higher for Angina
- 36% higher for Transient Ischemic Attack (TIA)
- 22% higher for Intracerebral Hemorrhage
- 35% higher for Subarachnoid Hemorrhage
In Conclusion
Overall, this study found vitamin D deficiency was significantly associated with poor outcomes following hospitalizations for cardiovascular and cerebrovascular events. Vitamin D deficiency was also associated with an increased risk of discharge to non-home facilities and for severe or extreme disability following the event, compared to those without vitamin D deficiency. These associations remained after adjusting for other risk factors.
Should You be Getting More Vitamin D?
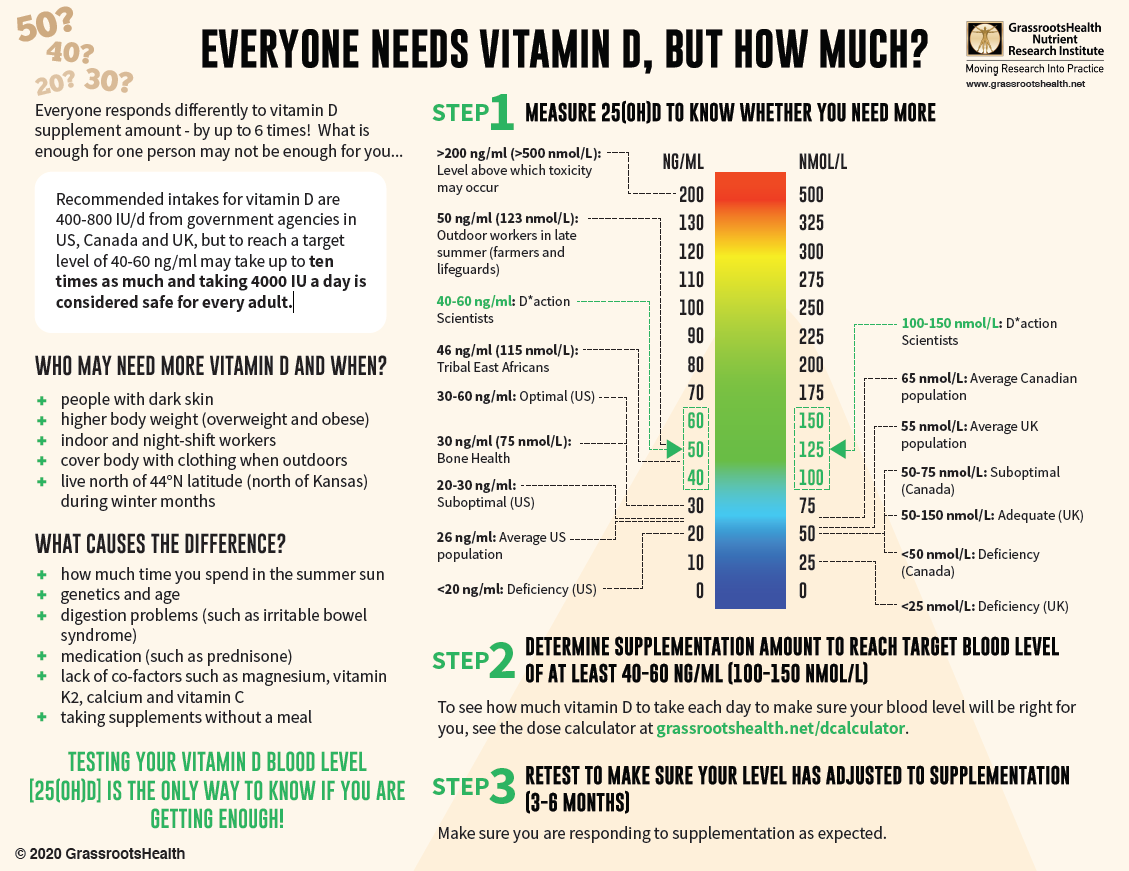
With almost 90% of the general population having vitamin D levels below the recommended 40-60 ng/ml (100-150 nmol/L), it is obvious that most people need more vitamin D. While most of us cannot achieve a vitamin D level of 40-60 ng/ml from sun alone, either due to our lifestyle, where we live, or other circumstances, we can certainly reach those levels with the right amount of supplementation.
Below is a guide for how much you might need, and who may need more. Your levels can be tested safely at home – order your home test kit today.
By joining the GrassrootsHealth projects, you are not only contributing valuable information to our study, but you are also gaining knowledge about how you could improve your own health through measuring and tracking your nutrient status, and educating yourself on how to improve it. Do you know what your status of vitamin D, omega-3s, and other essential nutrients is? Could your levels be improved? Test now to find out!