Published on April 9, 2019
We are often asked, “If I eat a healthy diet, can’t I get enough vitamin D from food alone?”. Our response is “Generally, no – most people will need to supplement to reach the recommended 40-60 ng/ml range.”
Can we solve the vitamin D deficiency through food?
 For most societies, food is not the primary source of vitamin D.
For most societies, food is not the primary source of vitamin D.
The National Institutes of Health (NIH) recommends 600 IU/day of vitamin D for anyone 1-70 years old and 800 IU/day for those over 70. However, this recommendation is based on maintaining bone health with a 25(OH)D concentration of 20 ng/ml, and does not consider any other health benefits of vitamin D. With a diet of vitamin D-rich fatty fish, eggs, and meat, together with fortified food sources of milk, orange juice, and cereals 600 IU/day is possible, but may not be enough vitamin D for some people to reach 20 ng/ml (much less the 40-60 ng/ml recommended by the GrassrootsHealth panel of scientists). Read the NIH Fact sheet on vitamin D to learn more about how the government views vitamin D and food.
Your Data Your Answers – What did we find?
In an earlier version of the GrassrootsHealth D*action questionnaire than what you see today, there was a larger section on diet. We used data from this section for 780 non-supplement taking participants, aged 16 years or older, to analyze food sources of vitamin D. This group had a mean serum 25(OH)D of 33 ng/ml, a mean age of 48 years, and 65% were female.
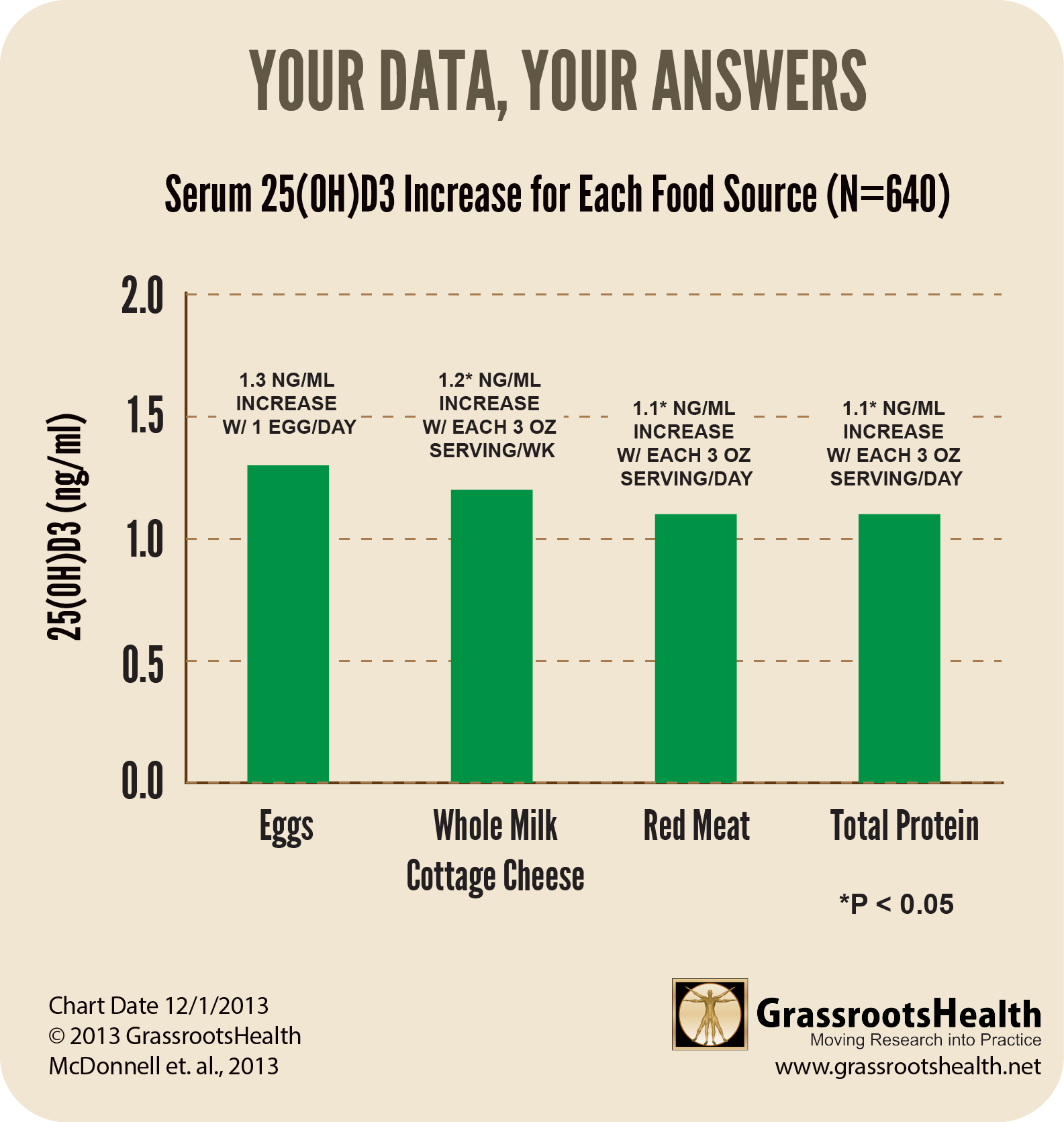
Foods that had an impact on vitamin D levels were whole milk cottage cheese, eggs, meat, and total protein. We found that vitamin D levels rose by about 1 ng/ml for each daily serving of eggs, meat, and total protein. For each weekly serving of whole milk cottage cheese, serum 25(OH)D rose by about 1 ng/ml.
Neither fish nor milk – both considered traditional food sources of vitamin D – was positively associated with vitamin D serum level in this cohort. Other foods that did not seem to make a difference were butter, fruits/vegetables, olive oil, mayonnaise, cream cheese, or sour cream.
Since milk is fortified, shouldn’t it have an impact on vitamin D levels? Yes, it should, but we may not have had enough milk drinkers in our group to show that impact. The milk consumption of the D*action cohort was very low, with an average of only 2 servings per week.
More on Milk – benefit in greater than one serving/day
Susan Whiting, who presented a webinar with GrassrootsHealth on Addressing Vitamin D Deficiency through Food Fortification, participated in an analysis of milk consumption and vitamin D status of Canadians which found that frequency of milk consumption did indeed have a positive effect on 25(OH)D concentrations. Those who consumed milk more than once a day had a mean 25(OH)D concentration of 30 ng/ml whereas those who consumed it less than once a day had a mean concentration of 25 ng/ml (view paper for detail). The analysis also found that the percentage of people who consume milk more than once a day is highest in children ages 6 – 11 years (the youngest age group of the study), at about 65%, and declines with age to just over 20% in seniors aged 60 to 79 years.
Does Food provide most of the basal vitamin D input in the US?
A paper by Robert Heaney et al., All-Source Basal Vitamin D Inputs Are Greater Than Previously Thought and Cutaneous Inputs Are Smaller, analyzed 8 studies with a total sample size of 3,000 individuals. The purpose was to try to determine the various sources of vitamin D input for non-supplement users. The findings included:
- All-source, basal vitamin D inputs are approximately an order of magnitude higher than can be explained by traditional food sources, an average of 2,000 IU/day.
 Vitamin D produced from sun exposure accounts for only 10-25% of unsupplemented input at the summer peak. This suggests that while sun exposure may have been important for synthesis of vitamin D under ancestral conditions, it is not playing a very large role in the vitamin D status of many first-world populations today.
Vitamin D produced from sun exposure accounts for only 10-25% of unsupplemented input at the summer peak. This suggests that while sun exposure may have been important for synthesis of vitamin D under ancestral conditions, it is not playing a very large role in the vitamin D status of many first-world populations today.- The remainder, approximately 1,600 IU/day, must come from undocumented food sources, possibly from meat and poultry, and possibly, in part, as preformed 25(OH)D.
Conclusion
While certain food sources can contribute significantly to vitamin D status, it is likely that vitamin D supplementation will remain key to improving vitamin D status at a population level.
How can I track my Vitamin D intake and status?
To help you track your Vitamin D and many different health outcomes, GrassrootsHealth has created an online tracking system called myData-myAnswers. You can also track your omega-3 and essential element levels as well as your pain, weight and colds, and any other custom item, such as your intake of certain foods, to see how your nutrient status and intake may be affecting your overall health. Check it out today!


 Vitamin D produced from sun exposure accounts for only 10-25% of unsupplemented input at the summer peak. This suggests that while sun exposure may have been important for synthesis of vitamin D under ancestral conditions, it is not playing a very large role in the vitamin D status of many first-world populations today.
Vitamin D produced from sun exposure accounts for only 10-25% of unsupplemented input at the summer peak. This suggests that while sun exposure may have been important for synthesis of vitamin D under ancestral conditions, it is not playing a very large role in the vitamin D status of many first-world populations today.



