Published on November 10, 2022
Is your vitamin D level lower than expected? One of these other nutrients could be to blame.
Key Points
- Poor magnesium status potentially impairs vitamin D metabolism, and deficiency may result in a vitamin D level that does not increase as much as expected in response to vitamin D supplementation; without sufficient magnesium, the amount of vitamin D that can be metabolized and used by the body is limited and may result in a lack of conversion of vitamin D into its other active forms
- Several studies have shown how magnesium intake affected the relationship between vitamin D and the risk of certain diseases; in one study, magnesium intake affected the association between vitamin D level and the incidence of type 2 diabetes, where the distribution of vitamin D levels between participants with or without type 2 diabetes was significant only in the high magnesium intake group
- Examples of other nutrients that seem to have an influence on vitamin D levels, based on data from the GrassrootsHealth D*action study, can be seen below as well

Previously, we have discussed how a lack of key vitamin D co-nutrients can keep vitamin D levels from rising. Co-nutrients are nutrients that work together for some process. If one co-nutrient is limited, either missing or not plentiful enough, then the process itself might also be limited. One key example is the relationship (or partnership) between vitamin D and magnesium.
Magnesium Supplementation and Status Affects Vitamin D
Magnesium is an important co-nutrient for vitamin D, and is involved in the biosynthesis, transport, and activation of vitamin D. Magnesium is the fourth most abundant mineral in the human body, however, an estimated 42% of young adults have ongoing magnesium deficiency. This can lead to problems with energy metabolism, muscle function, blood pressure regulation, insulin metabolism, cardiovascular function, nerve transmission, neuromuscular contraction, and more.
Studies have shown that poor magnesium status potentially impairs vitamin D metabolism, and an existing magnesium deficiency may result in a vitamin D level that does not increase as much as expected in response to vitamin D supplementation. As illustrated by Deng et al., without sufficient magnesium, the amount of vitamin D that can be metabolized and used by the body is limited and may result in a lack of conversion of vitamin D into its other active forms.
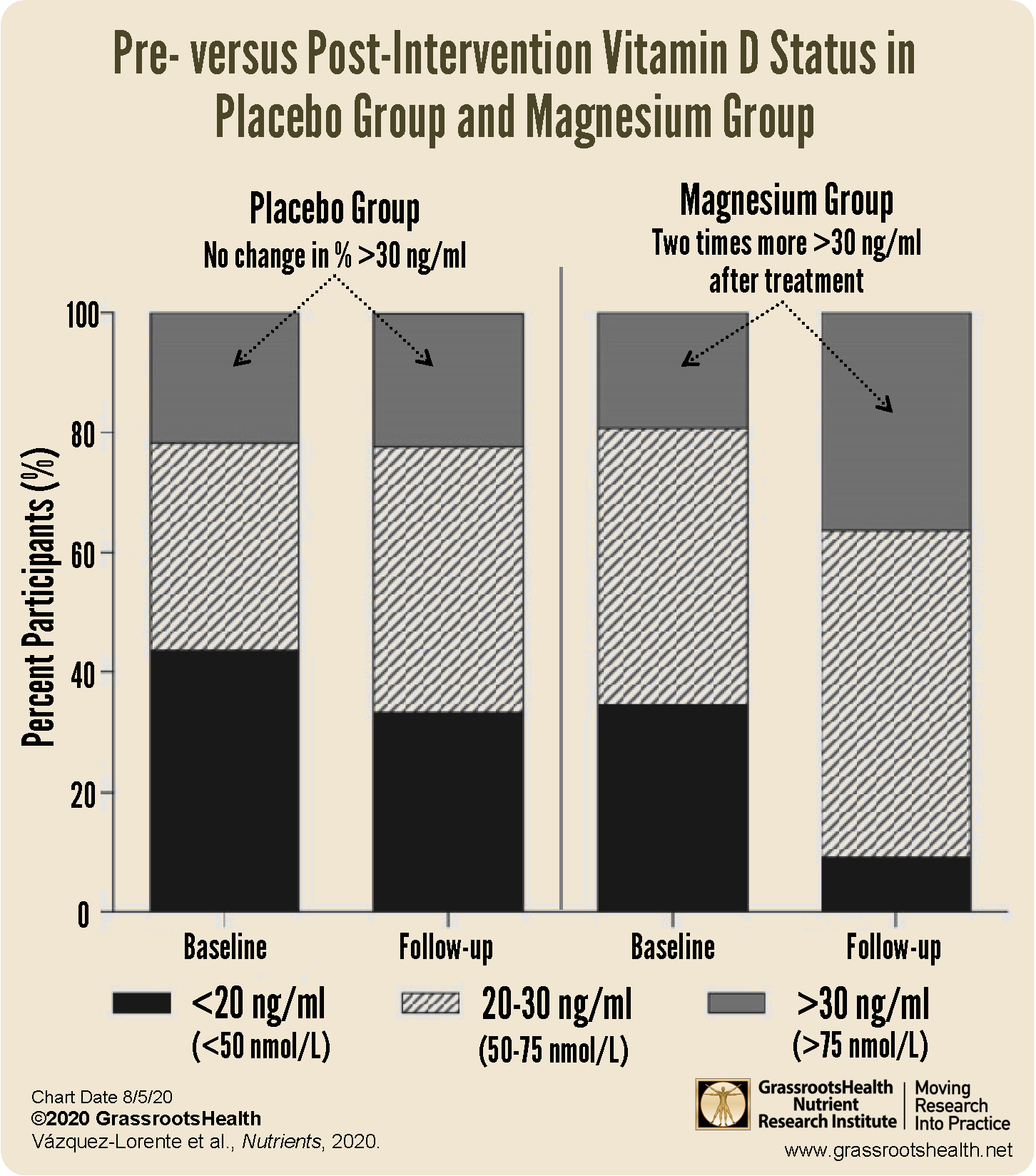
This was demonstrated in a study by Vázquez-Lorente et al., which looked at postmenopausal women to see if magnesium supplementation alone had an effect on vitamin D status. The vitamin D levels of 52 women between the ages of 44 and 76 years were tracked while the women were randomized into one of two groups: the Magnesium Group received 500 mg/day of magnesium for eight weeks, while the Placebo Group received a placebo. Note that over 40% of all women included in the study received less than two-thirds of the recommended intake of magnesium (320 mg/day) at the start of the study.
Approximately 80% of all women had vitamin D levels below 30 ng/ml at the start. By the end of the 8-week study, vitamin D levels increased significantly among the women in the Magnesium Group (p < 0.05), with a significant correlation between overall magnesium intake and resulting vitamin D level (p=0.03). After intervention, the percent of women below 30 ng/ml remained at 80% in the Placebo Group (no change), but was reduced to only 60% in the Magnesium Group (two times more women had vitamin D levels above 30 ng/ml).
Magnesium Intake Affects Association between Vitamin D and Disease Risk
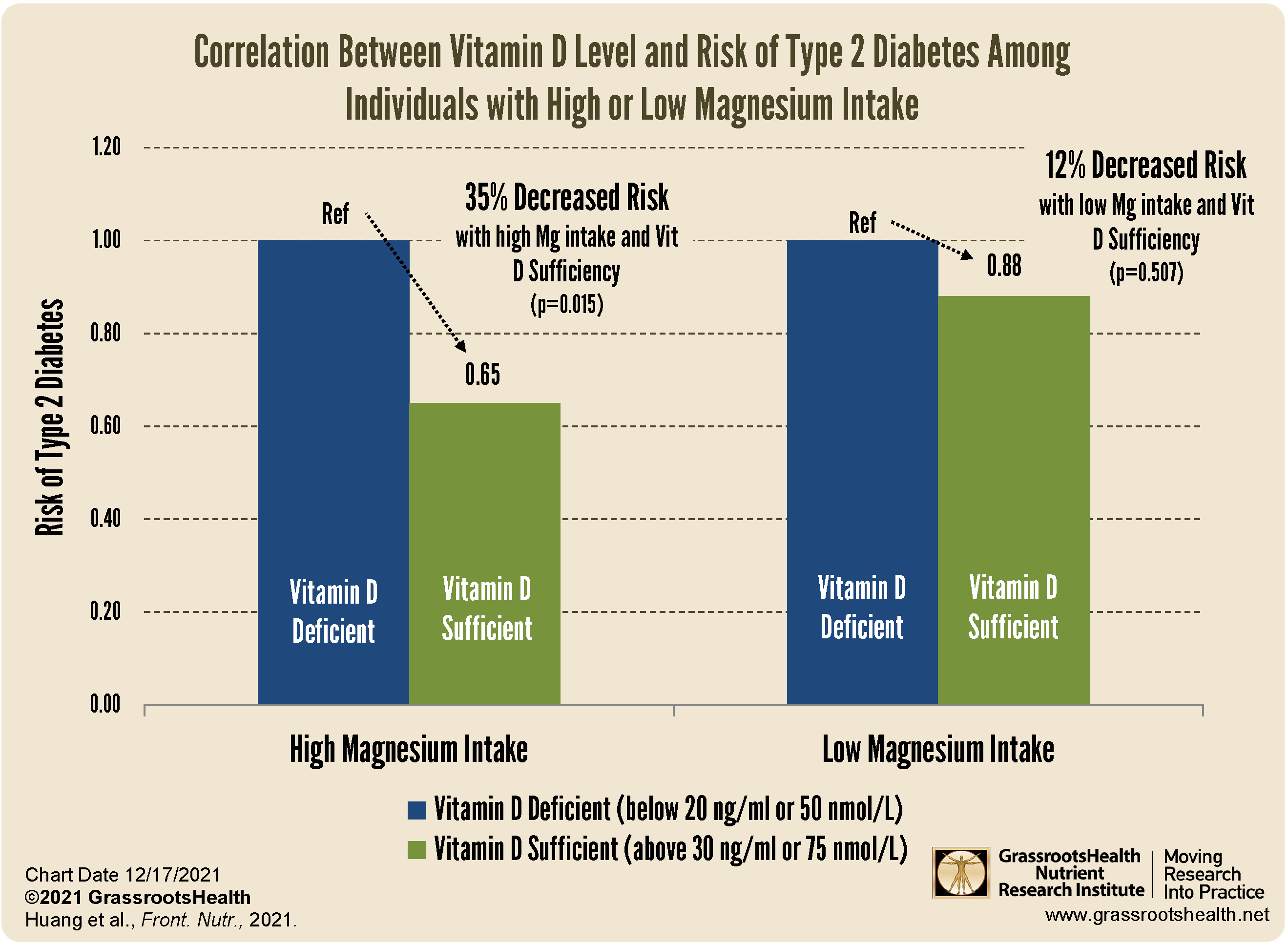
Several studies have shown how magnesium intake affected the relationship between vitamin D and the risk of certain diseases. Huang et al. completed a study that looked at whether the effect of vitamin D on the risk of type 2 diabetes differed based on a low versus a high magnesium intake. The authors found that magnesium intake affected the association between vitamin D level and the incidence of type 2 diabetes, where the distribution of vitamin D levels between participants with or without type 2 diabetes was not significantly different in the low magnesium intake group, but was in the high magnesium intake group.
In the group with high magnesium intake, there was a 35% significantly decreased risk of type 2 diabetes among the participants with vitamin D sufficiency compared to those with vitamin D deficiency, compared to the group with low magnesium intake, which only had a 12% non-significantly decreased risk among those with vitamin D sufficiency.
These studies clearly show the importance of getting enough magnesium with your vitamin D!
GrassrootsHealth Data Shows How Other Nutrients Affect Vitamin D Level
Some examples of nutrients that seem to have an influence on vitamin D levels, based on data from the GrassrootsHealth D*action study, can be seen below. On average, participants who had been supplementing with each of the nutrients listed below had a higher vitamin D level for any given vitamin D intake amount than those taking less or none. Visit this blog for details and charts on each of the nutrient relationships below.
Vitamin D Dose-Response by Magnesium and Vitamin K2 Intake
On average, those taking both supplemental magnesium and vitamin K2 have a higher vitamin D level for any given vitamin D intake amount than those taking either supplemental magnesium or vitamin K2 or neither. Specifically, 244% more supplemental vitamin D was needed for 50% of the population to achieve 40 ng/ml (100 nmol/L) for those not taking supplemental magnesium or vitamin K2 compared to those who usually took both supplemental magnesium and vitamin K2.
Vitamin D Dose-Response by Magnesium Intake
146% more supplemental vitamin D was needed for 50% of the population to achieve 40 ng/ml (100 nmol/L) for those not taking supplemental magnesium compared to those who took 400 mg/day or more.
Vitamin D Dose-Response by Vitamin K2 Intake
115% more supplemental vitamin D was needed for 50% of the population to achieve 40 ng/ml (100 nmol/L) for those not taking supplemental vitamin K2 compared to those who took 200 mcg/day or more.
Vitamin D Dose-Response by Calcium Intake
14% more supplemental vitamin D was needed for 50% of the population to achieve 40 ng/ml (100 nmol/L) for those not taking supplemental calcium compared to those who took 500 mg/day or more.
Vitamin D Dose-Response by Vitamin B6 Intake
63% more supplemental vitamin D was needed for 50% of the population to achieve 40 ng/ml (100 nmol/L) for those not taking supplemental vitamin B6 compared to those who took 20 mg/day or more.
Vitamin D Dose-Response by Vitamin B12 Intake
61% more supplemental vitamin D was needed for 50% of the population to achieve 40 ng/ml (100 nmol/L) for those not taking supplemental vitamin B12 compared to those who took 500 mcg/day or more.
Vitamin D Dose-Response by Vitamin C Intake
On average, those taking supplemental vitamin C in the amount of 1,000 mg/day or more have a higher vitamin D level for any given vitamin D intake amount than those taking less supplemental vitamin C. Specifically, 94% more supplemental vitamin D was needed for 50% of the population to achieve 40 ng/ml (100 nmol/L) for those not taking supplemental vitamin C compared to those who took 1,000 mg/day or more.
Vitamin D Dose-Response with Probiotic Intake
72% more supplemental vitamin D was needed for 50% of the population to achieve 40 ng/ml (100 nmol/L) for those did not take probiotics compared to those who did.
A Few More Vitamin D Co-Nutrients
A lack of other key vitamin D co-nutrients, such as calcium, boron and zinc, can reduce vitamin D absorption and production. On the other hand, a high intake of certain vitamins that compete with vitamin D, such as vitamin A in the form of retinol or retinyl palmitate (not beta-carotene), can cause a reduction in vitamin D levels. This form of vitamin A is found in food from animal sources (especially liver) and some supplements. Also, some medications including statins, prednisone and weight-loss drugs can block vitamin D.
Does Your Vitamin D Level Need a Boost from any of its Co-Nutrients?
 Having and maintaining healthy nutrient levels can help improve health, now and for your future. Choose which to measure, such as your vitamin D, omega-3s, and essential minerals including magnesium and zinc, by creating your custom home test kit today. Add hs-CRP to measure your level of inflammation as well. Take steps to improve the status of each of these measurements to benefit your overall health. You can also track your own intakes, symptoms and results to see what works best for YOU.
Having and maintaining healthy nutrient levels can help improve health, now and for your future. Choose which to measure, such as your vitamin D, omega-3s, and essential minerals including magnesium and zinc, by creating your custom home test kit today. Add hs-CRP to measure your level of inflammation as well. Take steps to improve the status of each of these measurements to benefit your overall health. You can also track your own intakes, symptoms and results to see what works best for YOU.
Enroll and test your levels today, learn what steps to take to improve your status of vitamin D (see below) and other nutrients and blood markers, and take action! By enrolling in the GrassrootsHealth projects, you are not only contributing valuable information to everyone, you are also gaining knowledge about how you could improve your own health through measuring and tracking your nutrient status, and educating yourself on how to improve it.