Published on January 5, 2024
An argument from a nurse’s eyes to update what is established, by Amanda Barber Alexander, MSN Ed, RN.
Key Points
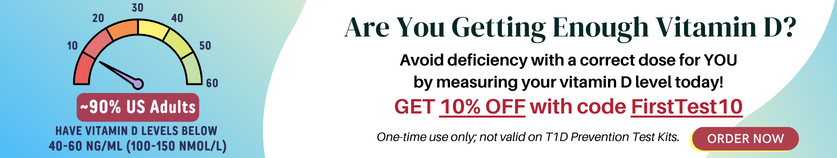
- While vitamin D is well known for its impact on bone health, its extra-skeletal effects are less known and infrequently taught on the world stage; subsequently, the importance of optimal vitamin D levels and the amount of supplementation necessary for health continues to be undisclosed in mainstream medicine
- Critical research findings show that only 1.7% of healthcare providers are appropriately trained to diagnose and manage vitamin D deficiency
- Sharing vitamin D education and new established guidelines within healthcare communities can establish solid professional preventative practices, while addressing a safe, effective, low-cost intervention that can make a big health impact
 Amanda Barber Alexander, MSN Ed, RN, is an Associate Professor of Nursing at Rasmussen University. She has 15 years of critical care and perioperative nursing. She participates in select nursing organizations and has been awarded two leadership certificates from the National Society of Leadership and Success. She has also received the Daisey Award for excellence in nursing. Amanda’s aspirations are to lead communities toward optimal health through research and education.
Amanda Barber Alexander, MSN Ed, RN, is an Associate Professor of Nursing at Rasmussen University. She has 15 years of critical care and perioperative nursing. She participates in select nursing organizations and has been awarded two leadership certificates from the National Society of Leadership and Success. She has also received the Daisey Award for excellence in nursing. Amanda’s aspirations are to lead communities toward optimal health through research and education.
Amanda has first-hand experience as a patient. For almost 5 years, she has been battling muscular weakness, fatigue, memory laps, and pain. She received a diagnosis of Fibromyalgia and muscle fatigue of unknown etiology. When Amanda started conducting vitamin D research with Dr. Beth Sanford, she realized she was a potential victim of vitamin D deficiency. She purchased a test kit from Grassrootshealth and it returned a critical low value. This was what she had been waiting for! It provided hope of a cure to her symptoms after 5 years of suffering, prescriptions, and continued illness. Now, Amanda is advocating for educating all healthcare providers on nutrient deficiency and appropriate testing.
Fun fact: Amanda spent 15 years bodybuilding and competing in the NPC and she looks forward to lifting again.
Vitamin D, “Are we current in our evidence-based practice?”
An argument from a nurse’s eyes to update what is established.
Vitamin D is well known for its impact on bone health; however, its extra-skeletal effects are less known and infrequently taught on the world stage. Recent research has identified noteworthy additional roles in physiologic homeostasis and pathologic processes such as DNA repair, gene expression, immunity, decreasing cancer cell proliferation, and lowering pro-inflammatory cytokines, among many others. Although these finding have been recognized, there is much controversy surrounding the amount of vitamin D needed to support these extra- skeletal effects. A review of these studies indicates the controversy is drawn from interpretations of studies of poor design. The failure and lack of consistent research methods has led to misinformation shared throughout medical communities. Subsequently, the importance of optimal vitamin D levels and the amount of supplementation necessary for health continues to be undisclosed in mainstream medicine.
In 2007, research completed by Dr. Micheal Holick stated that at least 1 billion people are deficient or insufficient in vitamin D worldwide (Holick, 2007). Almost twenty years have passed, and the number of individuals with vitamin D deficiency and insufficiency has remained the same. The absence of progressive education and guidelines for achieving and maintaining optimal vitamin D levels is identified as an impending issue for the medical community. Lack of vitamin D knowledge prohibits prevention and treatment of diseases and disorders of the cardiac, immunological, endocrine, brain, muscle, skin, reproductive and pulmonary systems. Conclusively, when providers understand the need to supply the body with enough vitamin D, they can intervene as necessary to help decrease future disease forecast and create cost-saving benefits for organizations and patients.
Provider Facts
A review of research literature shows that the knowledge and attitudes of healthcare providers decide their behaviors toward when and how to assess and treat vitamin D deficiency (Sanford BS, 2023). Critical research findings show that only 1.7% of healthcare providers are appropriately trained to diagnose and manage vitamin D deficiency (Rockwell, 2018). Additionally, Mekonnen et al. identified healthcare knowledge gaps in measuring and managing vitamin D deficiency across all provider continuums (Wubegzier Mekonnen, 2020). The findings clearly indicate a need for consistent recommendations and guidelines.
How current are vitamin D recommendations?
Vitamin D is obtained through sun exposure, certain foods, and supplementation. The evolution of societal practices in restricting sun exposure, increased consumption of process foods, and inadequate nutrient intake results in many people remaining deficient in vitamin D and in need of supportive supplementation. Vitamin D has two molecular forms delivered by food and dietary supplements. Ergocalciferol (Vitamin D2) and Cholecalciferol (Vitamin D3) are chemically different; vitamin D3 is the form the body makes and is recommended by professional medical organizations for supplementation. These organizations are responsible for decreasing health disparities by translating scientific discoveries and promoting evidence-based practice (Sanford BS, 2023).
A review of the professional organizations illustrates apparent variance in recommendations, especially where vitamin D is concerned. The variations confuse prescribers and decrease their confidence in screening and treatment of vitamin D deficiency. In 2011, the IOM established RDA (Recommended Dietary Allowances) for vitamin D specific to daily intake sufficient to maintain bone health and normal calcium metabolism in healthy people (NIH, 2023). The studies did not include individuals with other comorbid disease processes. Concurrently, the Endocrine Society set treatment and prevention guidelines that supported the IOM’s designation of 20 ng/ml vitamin D blood levels (measured as 25 hydroxyvitamin D) for bone health but suggested increased levels of 21-29 ng/ml as insufficient and recommended an aim for 30 ng/ml or higher for optimal overall health (Holick et al., 2011). Consequently, teams of researchers submitted follow-up recommendations for vitamin D supplementation. Most notably a team led by vitamin D scientist Dr. Michael Holick suggested recommendations include higher daily intakes for all age groups to maximize bone health and potentiate non-skeletal health benefits (Hollick et al., 2011). These debates over the correct amounts of vitamin D supplementation continue to this day and allude to a need for healthcare provider resources that establish safe and effective evidence-based vitamin D practices for optimal health.
Vitamin D Resources
Promotion of safe and effective vitamin D practice starts with disseminating current scientific findings and producing products that can be put into action. At GrassrootsHealth Nutrient Research Institute, educational tool kits have been designed with adaptable resources for use among front-line staff to address overall vitamin D knowledge deficits. A tool kit developed by Dr. Beth Sanford in collaboration with GrassrootsHealth supports efforts to promote healthcare provider knowledge and involvement in vitamin D evidence-based practice. The tool kit includes a vitamin D deficiency risk assessment quiz, an e-course, and a risk reduction plan. The self-paced e-course supplies an interactive experience. The developed questions challenge the reader to identify recommended best practice guidelines, and downloadable peer-reviewed articles and translation resources are included in the e-course as part of translating research to practice (Sanford BS, 2023). Finally, the vitamin D*calculator, which supplies updated recommendations for loading dose and maintenance doses needed for the serum 25 (OH) D levels, is easily accessible and user-friendly. Find these great resources @ Moving Research into Practice
Conclusion
Vitamin D is crucial for global disease prevention. Healthcare providers need clear, up-to-date vitamin D education and guidelines. Establishing localized resources for recommended daily allowances of vitamin D will reduce prescriptive related confusion. In addition, sharing vitamin D deficiency education and new established guidelines within healthcare communities can establish solid professional preventative practices, while addressing a safe, effective, low-cost intervention that can make a big health impact.
Test to See if You Are Getting Enough (or Too Much) Vitamin D and Other Important Nutrients
 Create your custom home test kit to measure your levels at home as part of the D*action project!
Create your custom home test kit to measure your levels at home as part of the D*action project!
With your kit you can measure your:
- Vitamin D
- Magnesium PLUS Essential and Toxic Elements
- Omega-3 Fatty Acids
- hsCRP
- HbA1c
- TSH
- Type 1 Diabetes Autoantibodies
Did you know that each of the above can be measured at home using a simple blood spot test? As part of our ongoing research project, you can order your home blood spot test kit to get your levels, followed by education and steps to take to help you reach your optimal target levels. Start by enrolling and ordering your kit to measure each of the above important markers, and make sure you are getting enough of each to support better mood and wellbeing!
Create your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. With measurement you can then determine how much is needed and steps to achieve your goals. You can also track your own intakes, symptoms and results to see what works best for YOU.