Published on June 26, 2017
Researchers in Tennessee knew that vitamin D deficiency could lead to chronic ailments, which in turn increases health care costs. The Veterans Administration is interested not only in the health of their veterans, but also in reduced costs associated with fewer visits to the VA, and lower incidence of disease.
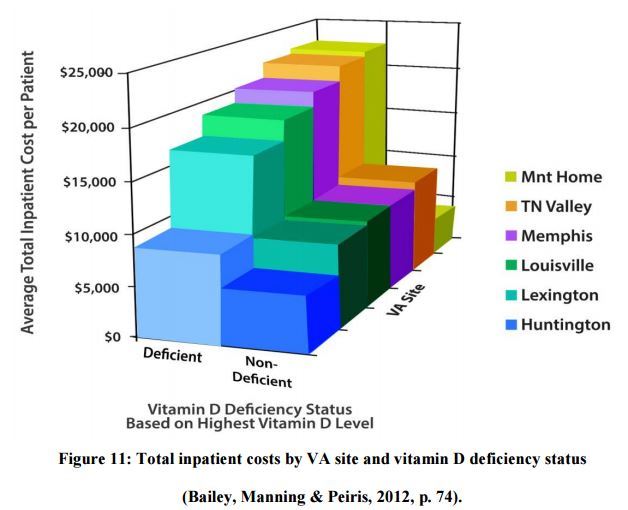
Without clear guidelines within the VA for vitamin D testing and monitoring, the researchers hypothesized that there would be differences in vitamin D testing, vitamin D status, and those differences would be associated with differences in overall health care costs. They looked at data from 6 different Southeastern VA Medical Center data where vitamin D testing had been in place from October 2004 to December 2008. This included 400,000 patients of which 15,340 had vitamin D tests within their records.
They defined vitamin D deficiency as 25(OH)D below 20 ng/ml (50 nmol/L).
What did they find?
For those patients with vitamin D test results, roughly 30-50% were vitamin D deficient on their initial test. The VA center with the lowest percentage of vitamin D deficiency also had more than 50% lower inpatient costs than the three centers with the highest rates of vitamin D deficiency. Also, patients who received one or more follow-up tests (which gives the patient data required to maintain their optimal vitamin D level) had 50% lower inpatient laboratory and pharmacy costs, as compared to those that only received one test.
They also measured what they called service utilization, which included the number of hospitalizations and the length of those hospital stays. Presumably, the healthier the person, the shorter their stay in the medical center. They found deficient patients were not only more likely to have an inpatient stay, but also to have a longer stay than their sufficient counterparts.
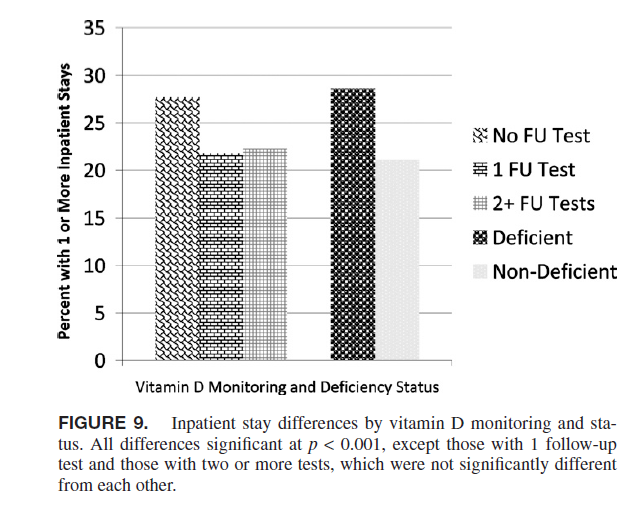
They compared patients who were both deficient and never had a follow-up test with those who were only deficient or had no follow-up test and those who were both sufficient and had at least one follow-up test. The former group had 70% higher total inpatient costs than the middle group, and almost 300% higher costs than the latter group. It is best to be sufficient, but what is also important is to get follow-up tests so that you can determine if what you are doing is working.
Conclusion
While the study focuses on testing, which we agree is very important, they also come up with a conclusion that they support the Endocrine Society’s recommendation on daily dosing (1000-2000 IU/day) over that of the NIH (600 – 800 IU/day, depending on age).
They also proposed that as a standard practice, vitamin D levels should be checked once or twice a year until their vitamin D levels are stable at the desired level.
“We recommend protocols that recognize site differences and facilitate testing and monitoring of vitamin D levels, especially in high-risk groups of veterans.”
GrassrootsHealth believes this should be applied to all populations, and has worked with institutions to implement with pregnant women through our Protect our Children NOW! nutrient field trial.
Resources
Vitamin D Testing Patterns Among Six Veterans Medical Centers in the Southeastern United States: Links With Medical Costs
Beth Bailey et al.
Military Medicine
2012
Read Paper
VitaminDWiki
Contains VA study, resulting PhD dissertation, and many others
Read Referenced Page