Published on August 3, 2017
Is Breastmilk Broken?
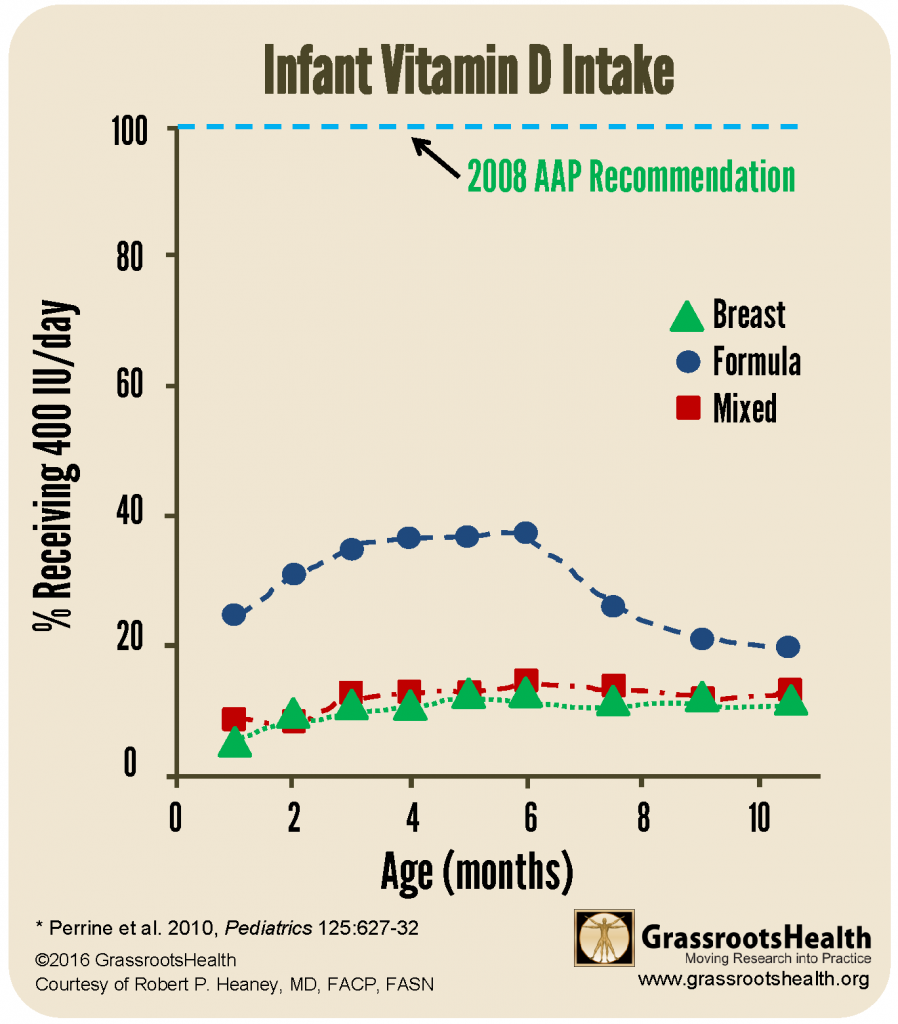
It is well-known that most breastfeeding babies are not getting adequate vitamin D and if a mother were to bring this topic up during a baby’s well-visit, the pediatrician would most likely recommend a 400 IU/day infant drop. This is fine and will work for the baby, but NHANES data has found that only 2-19% of all babies are actually getting the prescribed daily amount of vitamin D. That leaves over 80% not getting the recommended amount of vitamin D.
Is there another way? If breastfeeding is nature’s method for feeding babies, was it always flawed? Probably not, research on ancestral levels of vitamin D shows that pregnant mothers in ancestral tribes of East Africa have higher vitamin D levels during pregnancy.
But, we are not outdoors hunting and gathering daily – so how can nursing mothers in the modern world take care of BOTH themselves and their baby? Is there an ideal amount of supplement a nursing mother could take that would be helpful not only for herself but also provide an amount sufficient for the baby?
The result = 6400 IU / day.
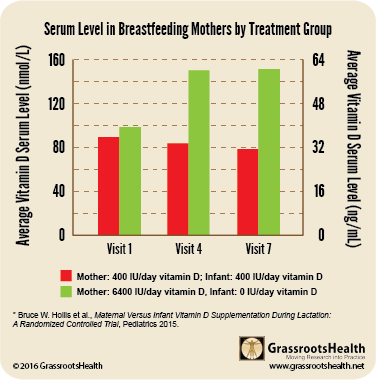
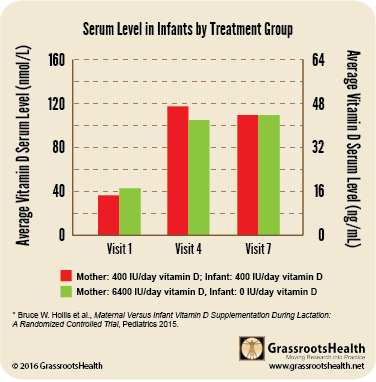
Please read on to fully understand the results, but the conclusion was 6,400 IU vitamin D /day gave mothers an average vitamin D level of 60 ng/ml (150 nmol/L) and gave babies the equivalent of 400 IU vitamin D/day – and an average vitamin D level of 40 ng/ml (100 nmol/L). This worked for the study as a whole, but there is a six-fold variability in how people respond to supplementation, so it is always better to test, not guess, and maintain the right vitamin D blood level – not just take a set amount of supplement. (Learn the health benefits to both mother and baby with vitamin d sufficiency.)
Description of Clinical Trial
This randomized controlled trial (RCT) divided the breastfeeding women/infant pairs, at 4-6 weeks post-partum, into one of three groups:
- Mother takes 400 IU/day vitamin D (placebo and prenatal vitamin with 400 IU), infant supplements with 400 IU/day vitamin D (1 drop liquid suspension).
- Mother takes 2400 IU/day vitamin D (2000 IU and prenatal), infant takes no vitamin D supplementation (placebo liquid drop). (This group was canceled about 4 years into the study due to an increase in infant vitamin D deficiency (defined as 25(OH)D < 20 ng/ml)).
- Mother takes 6400 IU/day vitamin D (6000 IU and prenatal), the infant takes no vitamin D supplementation (placebo liquid drop).
Previous research found that if the breastfeeding mother was only taking the recommended daily allowance of 400 IU per day, then an infant, solely fed on breast milk, would get the equivalent of 33 – 68 IU vitamin D / liter, which would provide the infant with far less than the recommended 400 IU/day. Hollis was a co-author in a study (2006) that reported infants breastfed by mothers taking only 400 IU/day typically had vitamin D levels < 5 ng/ml (< 12.5 nmol/L).
Current Status of Babies Today
Even though the American Academy of Pediatrics recommends supplementing infants with vitamin D right after birth, studies show a compliance of between 2 – 19%. Hollis calls infant supplementation “a largely failed initiative.”
Below is a chart of NHANES data (2009-2012) from the paper, Adherence to Vitamin D Recommendations Among US Infants Aged 0 to 11 Months, NHANES, 2009 to 2012
How do we get these babies the vitamin D they need?
This RCT concluded that giving breastfeeding mothers 6,400 IU vitamin D /day, and no additional supplement for the infant, made sure the mother became sufficient (with an average vitamin D level of around 60 ng/ml) AND infants became sufficient (with an average vitamin D level a little above 40 ng/ml). The infants in this group had equivalent vitamin D status to those who received 400 IU/day (and the mother also received 400 IU/day). Many other measurements and blood tests were taken, including weight, length and head circumference of the infant, which were similar for both groups.
6400 IU vit D/day = Sufficient mother AND baby
Summary
WHAT’S KNOWN ON THIS SUBJECT: The vitamin D concentration in breast milk of women taking 400 IU vitamin D per day is relatively low, leading to vitamin D deficiency in breastfeeding infants. As a result, the American Academy of Pediatrics recommends breastfeeding infants supplement with vitamin D within days after birth.
WHAT THIS STUDY FOUND: Maternal vitamin D supplementation alone with 6400 IU/day safely supplies breast milk with adequate vitamin D to satisfy the requirement of her nursing infant and offers an alternate strategy to direct infant supplementation
Daily intake is most important
One of the most important takeaway messages from this research is that breast milk can be an adequate source of vitamin D for the infant if the mother takes enough of a supplement daily! (Adequate daily sun exposure would also have the same result, but that was not part of this research study.)
In earlier research, Hollis analyzed how vitamin D is transferred from the mother to the baby and found that it is transferred primarily in its parent form as vitamin D3 rather than 25(OH)D, the compound that is most commonly measured in blood. Vitamin D3 has a half-life of approximately 12 – 24 hours, and thus has to be replenished daily; 25(OH)D has a half-life of approximately 3 weeks, so while intermittent dosing can maintain high levels of 25(OH)D, it will not be adequate for transferring the daily requirement of vitamin D3 to the breastmilk.
Hollis recommends the standard of care for breastfeeding mothers to be 6,400 IU vitamin D / day. This is safe and effective and ensures both mother and baby will become vitamin D sufficient.
References
Maternal Versus Infant Vitamin D Supplementation During Lactation: A Randomized Controlled Trial
Bruce W. Hollis et al.
Pediatrics
October 2015
Read Paper
Vitamin D deficiency in breastfed infants in Iowa
Ziegler EE et al.
Pediatrics
August 2006
Read Paper
Relationships among vitamin D, 25-hydroxyvitamin D, and vitamin D-binding protein concentrations in the plasma and milk of human subjects
Bruce W. Hollis et al.
The Journal of Clinical Endocrinology & Metabolism
January 1986
Read Paper
Adherence to Vitamin D Recommendations Among US Infants Aged 0 to 11 Months, NHANES, 2009 to 2012
Katherine A. Ahrens et al.
SAGE Journals
June 7, 2015
Read Paper