Published on May 5, 2022
Regular, safe sun exposure, where the number 1 rule is don’t burn, puts emphasis on skin type to help maximize the health benefits while minimizing the risks associated with sun exposure
Key Points
- While the body does have built-in mechanisms to help protect against UV damage, excessive UV exposure can result in skin issues such as actinic keratosis, cancers, wrinkling (which happens when UVA radiation damages the elastic tissues), and other skin problems; excessive sun exposure leads to sun burns, therefore the number one rule is “Don’t Burn!”
- Melanin is a pigment found in higher concentrations in darker skin; it has antioxidant and scavenging properties, and acts as an effective sunscreen by protecting skin cells (malanocytes and keratinocytes) from UV induced DNA damage. When utilizing safe UVB exposure to generate a tan, your outermost layers of the skin will make melanin and vitamin D, both of which protect against UV damage and resulting skin cancer.
- The balance of benefits and harms in response to sun exposure differs by skin type; those with darker skin are at lower risk for skin cancer but higher risk of vitamin D deficiency, while those with lighter skin have a higher tendency to burn and a higher risk of skin cancer, yet sun avoidance will require vitamin D supplementation
 Current public health recommendations advise against sun exposure because it has been associated with an increased risk for skin cancer. While true for people with fair skin and a history of repeated sun burns, for the majority of the population, sensible sunshine exposure (in proper doses, without burning) has a positive impact on health and may protect against disease, even helping people live longer.
Current public health recommendations advise against sun exposure because it has been associated with an increased risk for skin cancer. While true for people with fair skin and a history of repeated sun burns, for the majority of the population, sensible sunshine exposure (in proper doses, without burning) has a positive impact on health and may protect against disease, even helping people live longer.
To safely reap the health benefits from sunshine exposure, it is essential to understand what excessive exposure is, the possible harms of excessive UV exposure, and how to avoid them. Some of the many positive effects from sunshine exposure include the stimulation of anti-oxidant, anti-inflammatory, and immunosuppressive pathways which are helpful in many diseases. Unfortunately, some of the negative effects of chronic, prolonged UV radiation (the kind that leads to acute sunburn) includes damage to the skin cell DNA, inflammation, and photo-aging, as well as the initiation and development of certain skin cancers, which results from DNA that is not properly repaired after UV damage.
What Happens to Skin Cells Upon UV Exposure?
While the body does have built-in mechanisms to help protect against UV damage, excessive UV exposure can result in skin issues such as actinic keratosis, cancers, wrinkling (which happens when UVA radiation damages the elastic tissues), and other skin problems. This video clip from a seminar presentation by Dr. Michael Holick helps explain:
Clip starts at 7:20 – How does the skin respond to sunlight?
7:34 – Tanning and melanin, natural sun protection
11:20 – Damaging effects of excessive sun
12:08 – Beginning of historical perspective of sun
(keep watching from here for more great information!)
It is essential to remember this one very important point made by Dr. Holick – Excessive sun exposure leads to sun burns, therefore the number one rule is “Don’t Burn!”.
Tanning: Natural Protection from Sun Burn and Skin Cancers?
“Skin pigmentation is an indispensable photoprotective factor.” (Rai et al., 2022)
As Dr. Holick discusses in the video above, one of the molecules that is most protective in the skin is melanin, which (interestingly) is produced by both our own cells and by the microbes on the skin’s surface upon UV exposure. Melanin is a pigment found in higher concentrations in darker skin; it has antioxidant and scavenging properties, and acts as an effective sunscreen by protecting skin cells (malanocytes and keratinocytes) from UV induced DNA damage. This is one reason individuals with darker skin are at a lower risk for skin cancers – because they have more melanin and are therefore less likely to burn.
While the amount of melanin in your skin is primarily genetic, it can also gradually increase through sensible sun exposure (aka safe, non-burning tanning). When utilizing safe UVB exposure to generate a tan, your outermost layers of the skin will not only make melanin, but also vitamin D, both of which protect against UV damage and resulting skin cancer. Studies have shown that vitamin D produced in the skin can decrease DNA damage in the skin cells and facilitate DNA repair directly upon any UV damage, and help prevent cell death. A study by Rybchyn et al. showed that an adequate supply of vitamin D made available to the skin cells upon UVB exposure increases DNA repair and decreases unresolved damage, so that after 24 hours, DNA repair occurs and skin cells return to their pre-exposure state. The same observation has been made by Bolerazka et al., as the authors state “One of the demonstrated abilities of vitamin D is optimization of DNA repair, which protects against UV-induced mutations, the most common cause of skin cancer in humans,” with an important note about skin cancers, “The dominant risk factor is sunburn and not cumulative sun exposure.”
Amount of Risk is Highly Dependent on Skin Type
Another study by Shih et al. aimed to identify the levels of sun exposure that generated vitamin D with minimal skin damage, and found that both vitamin D and DNA damage were produced across all skin types, however, the depth of DNA damage within the skin differed by skin type. Those with the darkest skin had DNA damage only in the surface layers of the skin whereas those with the lightest skin had DNA damage across all skin layers. The study went on to say “People with darker skin can be encouraged to use sub-sunburn UVR-exposure to enhance their vitamin D.”
A recent webinar presentation by the World Health Organization highlighted this topic. Dr. Rachel Neale discussed the benefits of sunshine exposure, most notably the production of vitamin D, with an emphasis on how the balance of benefits and harms differs by skin type. She points out how those with darker skin are at lower risk for skin cancer but higher risk of vitamin D deficiency, while those with lighter skin have a higher tendency to burn and a higher risk of skin cancer, yet sun avoidance will require vitamin D supplementation. In this same presentation, Dr. David Whiteman helped to clarify why there is such a difference, stating that darker skin “renders an SPF equivalent to about 60 or more.” Could this indicate that, once lighter skinned people acclimatize their skin to the sun and develop a tan, their risk of sun damage could be reduced significantly?
The sun protection factor (SPF) of a natural tan is roughly equivalent to the actual protection of an SPF 50 sunscreen for an average user, considering most users apply only 25% of the recommended amount. Interestingly, scientists believe that skin pigment lightened as humans moved away from the equator to enable the body to make more vitamin D from locations that had less UVB available throughout the year.
Skin pigmentation has adapted to where people live for many generations, dark in the tropical plains, brown in tropical forests, progressing to very light at high northern European latitudes (Jablonski and Chaplin 2010, Jablonski 2021). In the tropical plain regions, the dark skin protects against free radical production, skin cancer, and folate destruction while still permitting sufficient vitamin D production. Outside the tropics in the northern hemisphere from the Middle East through northern Europe, skin has the ability to tan as solar UV exposure increases in spring and summer, resulting in about a four-fold reduction in UVB penetration.
A problem in the United States is that inhabitants with northern European ancestry may have skin pigmentation slightly lighter than appropriate for where they live, while inhabitants with African ancestry may have skin pigmentation darker than appropriate. As a result, pale-skinned inhabitants are more prone to skin cancer while dark-skinned inhabitants are more prone to vitamin D deficiency (Ames, Grant et al. 2021).
The DNA damage in the deeper layers for those with lighter skin may explain why those with a fair phenotype have higher skin cancer rates. The topic of melanoma risk upon UV exposure will be discussed in more detail in our next post.
What is Your Skin Type?
Since skin type influences sunburns and sunburns are associated with increased risk for skin cancers and melanoma, it is important to know your skin type to best personalize your sun exposure habits. The Fitzpatrick scale below classifies six skin types based on the response of different skin types to UV radiation.
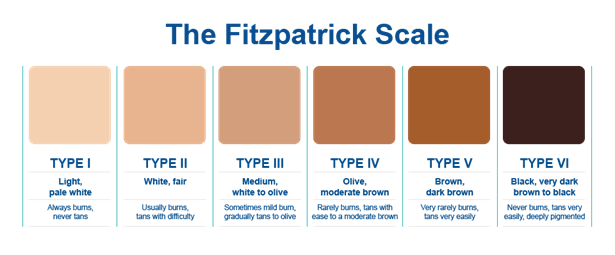
Credit www.perfectimage-llc.com
The amount of time spent in the sun can be personalized according to skin type and UV Index. Once you have identified your skin type, you can use tools such as the free dminder app to approximate how much time you can spend in the sun without burning. Whether or not you choose to use an app, it is important to allow skin to gradually acclimate to the sun, especially for those who spend a lot of time indoors, have lighter skin, after winter months, or during sun-seeking vacations. It is safer to increase exposure time gradually as this allows your skin to adapt to the sun’s intensity while safely producing a tan.
Are You Getting Enough Vitamin D? Measure Today!
 Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health now and for your future. Choose which additional nutrients to measure, such as your omega-3s and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. With measurement you can then determine how much is needed and steps to achieve your goals. You can also track your own intakes, symptoms and results to see what works best for YOU.
Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health now and for your future. Choose which additional nutrients to measure, such as your omega-3s and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. With measurement you can then determine how much is needed and steps to achieve your goals. You can also track your own intakes, symptoms and results to see what works best for YOU.
Enroll in D*action and Test Your Levels Today!