Published on November 16, 2023
What are the unique differences between each major form of vitamin D within the body, and under what circumstances might individuals consider measuring them? Part 3 of a series of questions and answers with Dr. Sunil Wimalawansa.
Key Points
- “Vitamin D” is a term that refers to several different compounds, most importantly: Vitamin D [as Cholecalciferol (D3)], 25-hydroxyvitamin D [25(OH)D or Calcifediol], and 1,25-dihydroxyvitamin D [1,25(OH)2D or Calcitriol]
- Peripheral target cells (such as immune cells) contain enzymes capable of converting vitamin D into 25(OH)D and then to 1,25(OH)2D to initiate a host of physiological functions critical to vitamin D’s roles in DNA regulation and interaction, and signal transduction
- The only form of vitamin D within the body that is, by definition, a hormone, is the portion of calcitriol that is secreted from renal tubular cells into the circulation, which then acts on distally located cells
- Outside of a few very specific situations and conditions mentioned, there is no value in measuring vitamin D, calcitriol, or any 24-hydroxy or other metabolites of vitamin D; serum 25(OH)D concentration is the only test a healthcare provider should request to establish the vitamin D status and correlate with diseases
 Dr. Sunil Wimalawansa has been researching vitamin D for over four decades. He is considered one of the world’s leading experts on micronutrients, especially vitamin D. His extensive background includes working with vitamin D in a laboratory setting, applying his vitamin D knowledge working with patients as a medical doctor, and directing clinical trials involving pharmaceuticals and vitamin D.
Dr. Sunil Wimalawansa has been researching vitamin D for over four decades. He is considered one of the world’s leading experts on micronutrients, especially vitamin D. His extensive background includes working with vitamin D in a laboratory setting, applying his vitamin D knowledge working with patients as a medical doctor, and directing clinical trials involving pharmaceuticals and vitamin D.
Today, we present Part 3 of this question-and-answer interview series with Dr. Wimalawansa, in which he shares his answers to questions regarding vitamin D3, 25(OH)D, and 1,25(OH)2D. We introduced Dr. Wimalawansa in Part 1 of this interview series, Vitamin D: Everything You Need to Know… and More, followed by Part 2, Defining Optimal Levels and Doses of Vitamin D for Every Individual.
We hope you have been enjoying this interview series and would like to extend a very big Thank You to Dr. Wimalawansa for sharing his knowledge and time with us! Stay tuned for Part 4, coming soon.
Introducing Today’s Topic
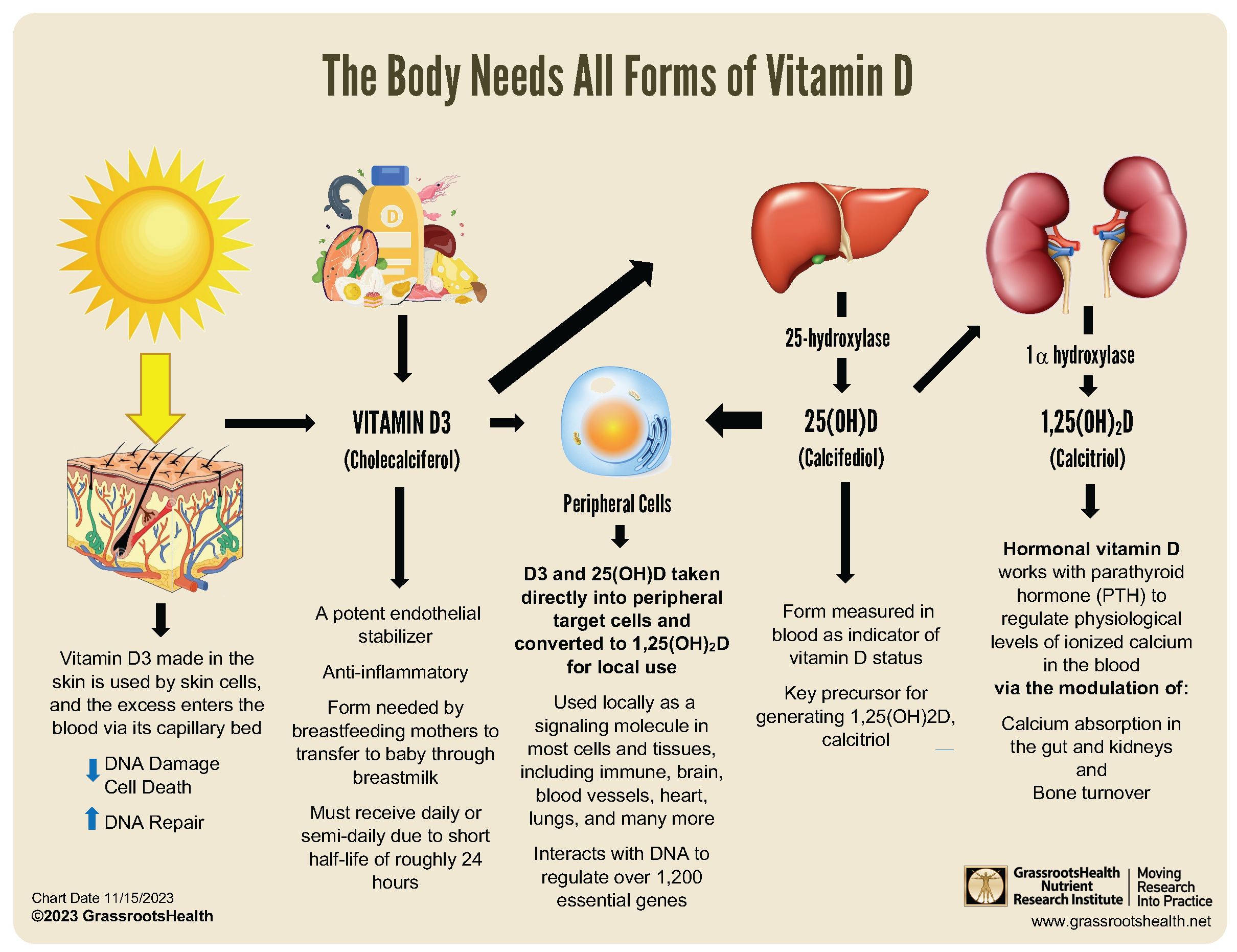
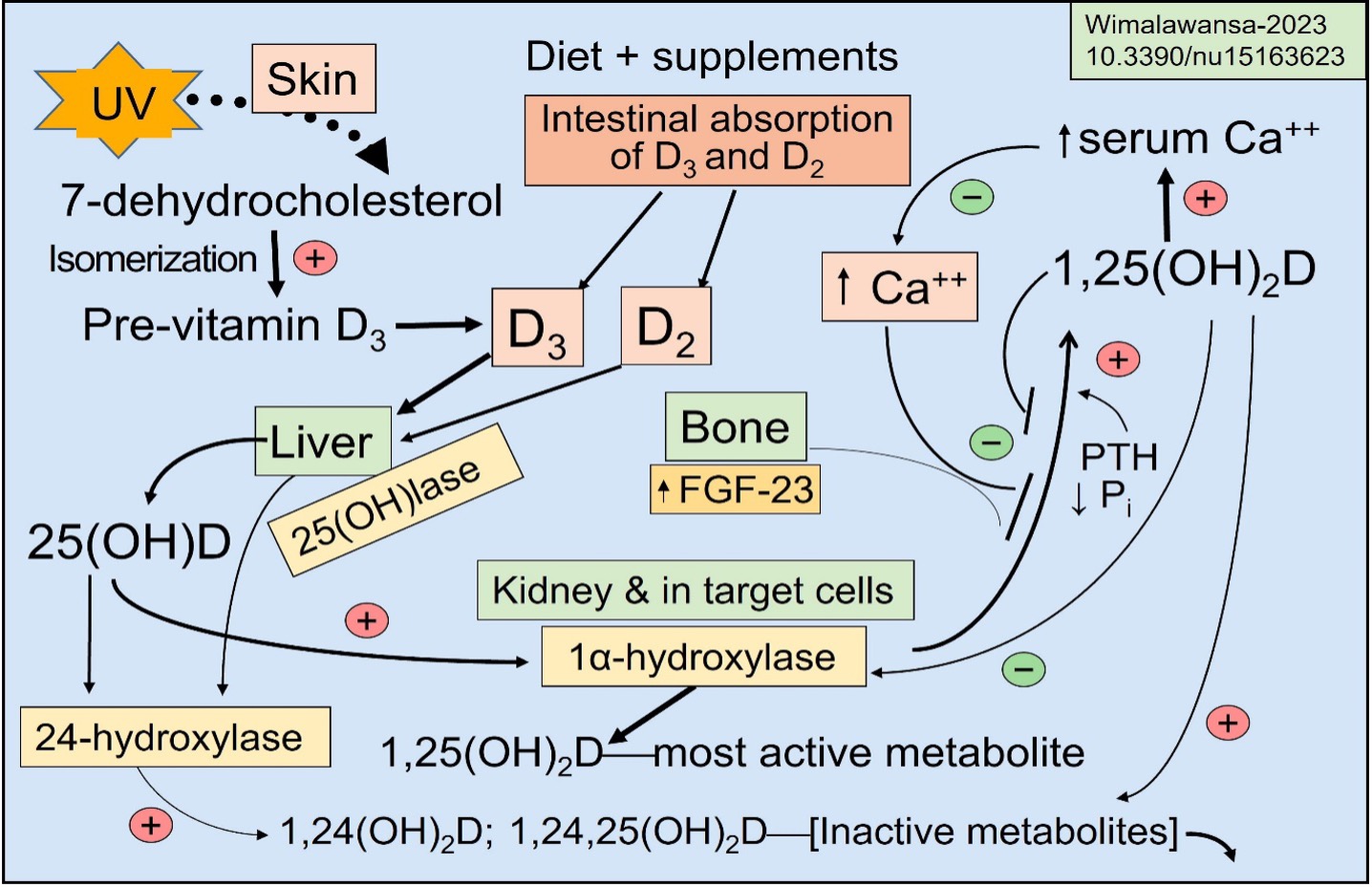
“Vitamin D” is a term that refers to several compounds. In this post, we will be discussing the three specific forms of vitamin D illustrated in the diagram below: Vitamin D [as Cholecalciferol (D3)], 25-hydroxyvitamin D [25(OH)D or Calcifediol], and 1,25-dihydroxyvitamin D [1,25(OH)2D or Calcitriol].
Note: Vitamin D2 (ergocalciferol) will not be discussed in this section, as it is a synthetic (non-human) product that is derived from plant precursors that is not utilized by the body as efficiently as vitamin D3. With a much shorter half-life, it remains in the blood for only a few hours. Supplementation with vitamin D2 will be discussed in more detail in the following post.
Questions and Answers with Dr. Wimalawansa
Can you explain how vitamin D is synthesized and circulated in the blood?
In humans, vitamin D3 is naturally obtained following exposure of the skin to the UVB range (between 280 and 305 nM) of sunlight; it converts an endogenous compound, 7-dehydrocholesterol, into previtamin D. It then isomerizes to form vitamin D3 and diffuses via capillary beds in the skin into the circulation (DOI: 10.1111/1523-1747.ep12479237). In addition to the liver, vitamin D is circulated to all other body tissues.
Peripheral target cells for vitamin D contain both 1α-hydroxylase and 25-hydroxylase enzymes capable of converting vitamin D into 25(OH)D and then to 1,25(OH)2D to initiate a host of physiological functions (DOI: 10.1016/j.taap.2004.12.022) (DOI: 10.1210/jc.2013-2653). This “intracellular” generation of calcitriol in target cells like immune cells is critical for autocrine and paracrine functions of vitamin D and its DNA interactions (i.e., Genomic actions) that regulate over 1,200 essential genes (https://www.ncbi.nlm.nih.gov/pubmed/16886665) (DOI: 10.1016/j.abb.2012.01.013).
Could you explain what pro-drugs and pro-hormones are—Is vitamin D a pro-hormone?
The terminologies pro-hormone, pro-drug, and pro-biotic refer to compounds that are inactive when administered but become fully active when they split or cleave, releasing their active component, as in pro-insulin. Such a process does not happen in the activation of vitamin D. It is the same parent vitamin D molecule that gets hydroxylated (converted) to form 25(OH)D (calcifediol) in the liver. It then gets further hydroxylation in renal tubular and peripheral target cells to form 1,25(OH)2D (calcitriol)—the most active form. Therefore, VITAMIN D is neither a pro-drug, pro-hormone, nor hormone but is a vitamin.
Some say vitamin D is a hormone. Can you explain why this confusion?
Hormones are produced in a cluster of cells or an (endocrine) organ. The final product from these cells—the hormone—is secreted into the bloodstream and acts on cells located distally. Vitamin D is synthesized in skin cells following exposure to ultraviolet B (UVB) rays. 7-dehydrocholesterol is converted to pre-vitamin D and isomerized to form vitamin D within skin cells. “Vitamin D” does not bind to a receptor (receptors are a complex protein with an effector system generating signals) with high affinity and has no known endocrine functions. Therefore, vitamin D is not a hormone, and the skin is not an endocrine organ (DOI: 10.3390/nu15163623). The vitamin D metabolite that binds to a receptor is calcitriol. Although commonly, it is called a vitamin D receptor, it should be re-named as calcitriol receptor (CTR) (DOI: 10.3390/biomedicines11061542).
Vitamin D is a fat-soluble compound that cannot be freely transported in an aqueous solution like blood. Therefore, as with other lipid-soluble molecules, vitamin D (and also calcifediol and calcitriol) gets attached (binds) to vitamin D-binding protein (VDBP; a large protein in the blood), before they are released into the circulation. Vitamin D is predominantly transported to the liver, where 25-hydroxylation occurs to form 25(OH)D (calcifediol)—the precursor for 1,25(OH)2D (calcitriol). Vitamin D and 25(OH)D also get into peripheral target cells, which are hydroxylated to form calcitriol, as illustrated in the diagram above. Calcifediol is a vitamin D metabolite but not a hormone (DOI: 10.3390/ nu15173842).
Calcifediol that reaches renal tubular cells (kidneys) gets further hydroxylated at the 1α-position of its carbon rings, generating 1,25(OH)2D calcitriol. The portion of calcitriol that is secreted from renal tubular cells into the circulation then acts on distally located cells—thus, by definition, it is a hormone (DOI: 10.3390/nu15163623).
The portion of vitamin D and 25(OH)D that does not enter renal tubular cells is transported via circulation. It diffuses into peripheral target cells, like immune cells, prostate, colon, brain, breast, etc. Vitamin D and 25(OH)D convert directly within these cells (i.e., inside these cells) to form the non-hormonal calcitriol. This portion of calcitriol does not secrete back into the circulation; in these circumstances, it is not a hormone. Instead, once bound to the calcitriol receptors (CTR) in the cell, it acts on the genome to modulate DNA. Intracellular calcitriol is also a critical signaling molecule, initiating autocrine/intracrine and paracrine functions (of vitamin D) within those cells. This portion of non-hormonal vitamin D is critical for the genomic and some non-genomic functions of vitamin D. (DOI: 10.1016/j.jsbmb.2006.12.078)
During genomic and metabolic activities and autocrine/intracrine and paracrine signaling processes, calcitriol, magnesium, and other cofactors get consumed (DOI: 10.3390/nu15173842). Therefore, these cells need a continuous supply of micronutrients, particularly vitamin D and magnesium, for proper physiological functions.
Vitamin D metabolites are mostly inactivated by the 24-hydroxylase enzyme (generated from the CYP24A1 gene), converting them to inactive 24-hydroxylated metabolites. The following diagram explains the generation of vitamin D and its metabolic activities (DOI: 10.3390/nu15163623).
I hope this simplified rationale is sufficient to understand that vitamin D is a vitamin, not a hormone. Note that politicians and regulators are eager to falsely re-categorize vitamin D as a hormone, despite it being a nutrient (e.g., this was already attempted by New Zealand’s health department in 2022). Their goal is to regulate and control vitamin D.
Such would take away the over-the-counter availability of this nutrient to the public. If this is the case, vitamin D use will dramatically reduce, significantly increasing sicknesses and healthcare costs. All for the financial benefit of bureaucrats and politicians and profiting big pharma—as with other medications and hormones. Government agencies should never be allowed to regulate any micronutrients, including vitamin D, making them pharmaceuticals. It is all about money, control, and power—nothing concerning science and humanity.
Can vitamin D3 be metabolized within cells or tissues outside the liver?
Yes—as mentioned above, a portion of both vitamin D3 and 25(OH)D that does not enter the renal cells diffuses into peripheral target cells for local conversion and use. Most cells and tissues in the body have the enzymes needed to make 1,25(OH)2D (the same molecule that acts as a hormone)—the calcitriol receptor need to use 1,25(OH)2D for its biological activity. These cells will pull the available vitamin D3 AND 25(OH)D from the blood into the cell and convert it into 1,25(OH)2D. This intracellularly generated calcitriol acts directly within the cell to meet several needs. Consequently, low calcitriol generation or receptor abnormality causes serious diseases in humans.
In this way, 1,25(OH)2D plays an important role in gene expression. This calcitriol component that is generated within those cells allows access to the cell’s DNA and modulates specific genes (can be turned on or off) in response to signals that the cell receives from its membranes and via cytokines, allowing proper responses to its needs and demand. When there is not enough vitamin D or 25(OH)D present in the blood, there will not be sufficient conversion of vitamin D and 25(OH)D to 1,25(OH)2D within these cells, leading to inefficient gene expression and a sub-optimal cellular response, therefore leading to ill-health. (DOI: 10.1016/j.jsbmb.2006.12.078)
Why is daily and weekly vitamin D administration better than less frequent administration, like once every three months?
We are supposed to obtain vitamin D from sun exposure daily. Taking vitamin D3 supplements is the next best option when daily sun exposure is not possible. This keeps the blood levels of vitamin D and especially 25(OH)D concentrations steady without too much fluctuation—this is the physiological status.
Infrequent administration of high doses of vitamin D beyond once a month is generally unhelpful and could be counter-productive (https://www.grassrootshealth.net/blog/taking-vitamin-d-can-ineffective-possibly-harmful/). Therefore, a daily maintenance dose, or administration of 50,000 IU weekly (or every 10th day—three times a month) is the way to go. In addition, as we discussed, vitamin D and magnesium are consumed each day and need to be replaced. Considering these, a shorter duration of administration, like once a day (or once a week), is better.
Consumption of vitamin D within cells accelerates with illnesses, especially during infections. Therefore, as we discussed previously; even those with normal blood 25(OH)D levels should be supplemented daily with vitamin D (or calcifediol). Nevertheless, very few healthcare workers today engage with this best, highly cost-effective clinical practice that can shorten hospital length of stay, prevent intensive care admissions, complications, and deaths, and markedly reduce healthcare costs. Instead, everyone seems to want high-end, expensive medications and interventions but neglects the nitty gritty in preventive medicine that virtually costs nothing.
When vitamin D is consumed daily, vitamin D3 and its metabolite 25(OH)D are in equilibrium and relatively similar concentrations in blood. For most clinical purposes, including establishing a person’s vitamin D status, measuring serum 25(OH)D concentration (not calcitriol) is indicated.
Is measuring Vitamin D3 or 1,25(OH)2D clinically essential or valuable?
Let’s discuss the half-lives of vitamin D. This will help the audience understand the importance of daily (or weekly) vitamin D administration, especially during pregnancy and lactation. Half-lives of these three components in blood are different (see the table below) and vary from hours to weeks. Compared to calcitriol with short half-life, the blood concentration of calcifediol is stable and fluctuates less (see Table 1: DOI: 10.3390/nu14142997).
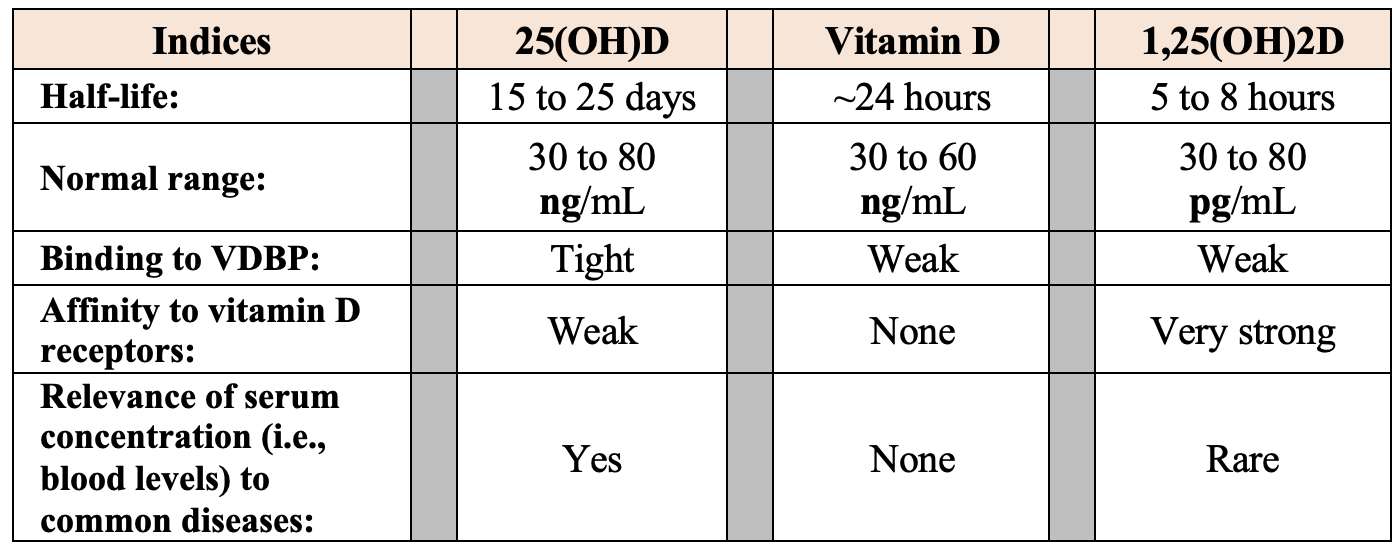
Note: The concentration of 25(OH)D (calcifediol) is about 900-fold higher than 1,25(OH)2D (calcitriol) (DOI: 10.3390/biomedicines11061542). At these very low concentrations, the circulating hormonal form of calcitriol is incapable of entering peripheral target cells like immune cells. Consequently, administration of calcitriol does not help in infections or autoimmune disorders; thus, it is not indicated.
There is no rationale for measuring vitamin D in the blood: its levels are clinically uninterpretable and do not correlate with health conditions. GPs and PCPs should only request measurements of 25(OH)D. The common causes of lower serum 25(OH)D include sun avoidance behavior, darker skin, higher latitudes, winter times, concomitantly taking catabolic drugs, and higher utilization during acute illness and infections. Serum 25(OH)D concentrations can be lower in hypothyroidism and with medications like anticonvulsants, anti-retroviral agents, impaired gastrointestinal fat malabsorption (e.g., with cholestyramine and orlistat), and gastric bypass surgery, and during acute illnesses and infections.
In conjunction with the calcitriol generated in the kidney, the PTH hormone primarily regulates circulatory calcium and phosphate. Circulating calcitriol is increased by PTH hormone arising from parathyroid glands [and also PTH-related peptide secreted by specific cancer cells], and high concentrations of some hormones (e.g., estradiol, testosterone, prolactin, and prostaglandin), whereas high corticosteroid levels decrease calcitriol levels. Measurement of calcitriol is restricted to parathyroid disorders, renal failure, and hypercalcemia.
Are there conditions requiring measurement of calcitriol in blood?
Calcitriol is measured primarily to diagnose “functional disorders” of the parathyroid glands, such as hyperparathyroidism, hypoparathyroidism, and pseudohypoparathyroidism. It is also measured in hypercalcemic conditions, renal osteodystrophy, and vitamin D-resistant rickets. Calcitriol levels are useful for differential diagnosis of hypercalcemia, to exclude squamous cell carcinoma from the head and neck region, and to exclude parathyroid disease, especially when the PTH-related peptide (PTHrp) measurements are unavailable.
Apart from the conditions mentioned above, blood levels of vitamin D and calcitriol are measured in research studies and not indicated in routine clinical setups. While the utility is low, the cost of their measurements is high. Such measurements are unjustified, except in a few uncommon conditions, not relevant in standard GPs and PCPs’ clinical practices. As mentioned above, half-lives of vitamin D and 1,25(OH)2D in circulation are short and fluctuate; thus, levels are unstable and inappropriate to measure. Besides, their interpretations are unreliable and hard to correlate in patients except for renal failure and hypercalcemia.
What are the specific indications for measuring calcitriol?
The most typical reason for measuring calcitriol in blood is to diagnose (or exclude) parathyroid disorders. Besides that, measurement of calcitriol is indicated in rare conditions like genetic abnormality of the CYP27B1 gene, which produces “1α-hydroxylase” (where calcitriol synthesis is decreased), as in vitamin D-dependent rickets and hypophosphatemic rickets (Type 1), AND vitamin D “receptor” gene abnormalities like vitamin D-dependent rickets (Type 2), in which calcitriol levels are increased. These disorders are extremely rare.
In persons with (usually incidental) findings of hypercalcemia, calcitriol is measured to narrow down the differential diagnosis to understand the reason for increased blood calcium levels (i.e., parathyroid origin vs. some other etiology)—calcitriol also could be high in granulomatous diseases, where it generated outside renal cells. Example of the latter are sarcoidosis, tuberculosis, and rarely in inflammatory bowel disease and rheumatoid arthritis. Measuring calcitriol is also indicated as a part of investigating hypercalcemia and vitamin D intoxication, which is exceedingly rare. Because the physiological feedback regulation of 1α-hydroxylase activity is absent in granuloma macrophages, they could synthesize larger amounts of calcitriol leaking into the bloodstream, causing hypercalcemia, a pathological situation.
In summary, outside the situations and conditions mentioned above, there is no value in measuring vitamin D, calcitriol, or, for that matter, any 24-hydroxy or other metabolites of vitamin D, including during nutritional assessments or therapy. Serum 25(OH)D concentration is the only test a healthcare provider should request to establish the vitamin D status and correlate with diseases.
Read Part 4 of this Interview Series: How Does One Determine the Right Amount and Type of Vitamin D to Take?.
* The above is a scientific discussion and should not be considered medical advice. Regarding clinical or personal issues, Prof. Wimalawansa advises readers to consult her/his physician.
Test to See if You Are Getting Enough Vitamin D and Other Important Nutrients
 Create your custom home test kit to measure your levels at home as part of the D*action project!
Create your custom home test kit to measure your levels at home as part of the D*action project!
With your kit you can measure your:
- Vitamin D
- Magnesium PLUS Essential and Toxic Elements
- Omega-3 Fatty Acids
- hsCRP
- HbA1c
- TSH
- Type 1 Diabetes Autoantibodies
Did you know that each of the above can be measured at home using a simple blood spot test? As part of our ongoing research project, you can order your home blood spot test kit to get your levels, followed by education and steps to take to help you reach your optimal target levels. Start by enrolling and ordering your kit to measure each of the above important markers, and make sure you are getting enough of each to support better mood and wellbeing!
Create your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. With measurement you can then determine how much is needed and steps to achieve your goals. You can also track your own intakes, symptoms and results to see what works best for YOU.