Published on August 30, 2018
Too much information
It is hard to know what to do with nutrient related information these days. Is it correct? Would it help your health condition? With any nutrient, including vitamin D, you could search the Internet and find several positive and negative articles on its effect.
One thing we know at GrassrootsHealth, is that there IS ENOUGH evidence on vitamin D to act. Vitamin D is essential for not only muscular/skeletal conditions but also immune function. Most likely if you are reading this, you believe the same thing – but how do you articulate this to others, or keep your faith, on the eve of published “bad” findings.
Scan for “tells”
Just as a poker player watches their opponents for tells, so should you scan the news article or research paper for these basic tenants of nutrient research, as outlined by Dr. Robert Heaney in his paper Guidelines for optimizing design and analysis of clinical studies of nutrient effects.
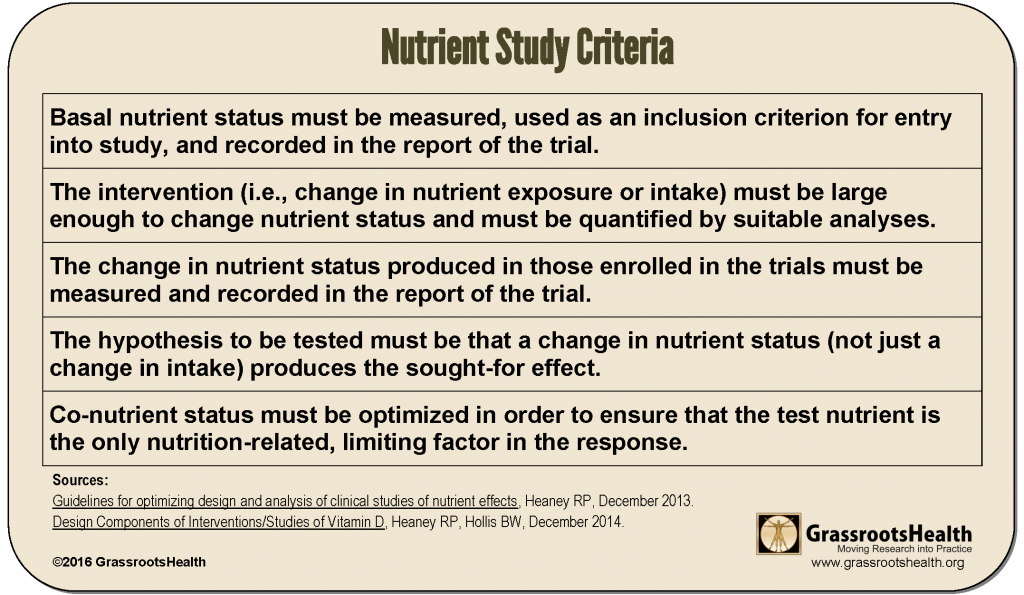
Be wary of findings from any clinical trial with these common problems
- Bolus dosing (generally large, intermittent dosing) – immune function only improves with daily dosing of vitamin D. Yet many studies on muscular/skeleton hypothesis were very effective on bolus (weekly, monthly) dosing.
- Hypothesis/goal does not mention change in nutrient status – this premise will be the core problem with items 4-6 below. Since vitamin D synthesis varies greatly for each person, the hypothesis cannot be by treatment amount (supplement intake) but instead needs to be investigated around achieving a certain serum level.
- No initial serum measurement – you can’t measure change if you don’t know the starting value.
- Participants are not deficient (<20 ng/ml) at the start – see Dr. Grant’s comment below. Since an effective study would change nutrient status significantly, the study needs at least one group to start at the low end.
- Low dosing (under 2,000 IU/day) – may not move nutrient status significantly for enough of the study participants to observe any effect.
- Analyzed only by dosage/treatment group, not by serum level – we need to know what serum level our patients should achieve for the desired effect.
- Less than or equal to 6 months testing for chronic conditions and disease prevention – as Dr. Holick says so eloquently below, it takes time to change nutrient levels within the body.
- No mention of co-nutrients, no attempt to optimize co-nutrients – this criteria is not a reason to throw out the study, but it would be optimal to optimize co-nutrients.
Below, some of the GrassrootsHealth Panel of Scientists speak to what they deem are some of the most important of the Heaney criteria.
Dr. Grant reminds us to check our assumptions
“Most vitamin D clinical trials were designed based on the guidelines for pharmaceutical drugs, rather than those for nutrients. Pharmaceutical drug trials assume that the trial is the only source of the agent and that there is a linear dose-response relation between agent and health outcome. Neither assumption is satisfied for vitamin D. Robert Heaney outlined the guidelines for nutrient studies in 2014 [Heaney, 2014]. One of the key points is that people enrolled in the studies should have low status of the agent of interest at the time of enrollment. Most vitamin D trials do not use that as a condition of enrollment. As a result, they mainly address the question: Does giving the average healthy population a modest amount of vitamin D reduce the risk of adverse health outcomes over a short time period? As shown by the analysis by Bolland [2011], the strongest effects will be found for those with low baseline vitamin D status. ”
William B. Grant, PhD
Sunlight, Nutrition and Health Research Center
San Francisco
Dr. Holick addresses the need for a significant change in nutrient status
– which doesn’t occur with paltry treatment groups (400 IU, 800 IU)
“It is remarkable to think that treating a person with a sub-optimal dose of vitamin D for a few years would overcome the consequences of a lifetime of vitamin D deficiency that has been associated with increased risk for many deadly cancers, cardiovascular disease, neurocognitive dysfunction and autoimmune diseases. These chronic illnesses likely were initiated many years before they become manifest. Most of the meta-analyses reviewed by the authors were studies that were relatively short term and used suboptimal doses of vitamin D.
Bottom Line: Meta-Analyses and rehashed meta-analyses, including this one [Allan, 2016], that are promoted in the lay press as new studies, demonstrating that vitamin D has little health benefit beyond musculoskeletal health needs more scrutiny. Vitamin D has existed on this planet for more than 500 million years. Our hunter-gatherer forefathers outside every day were likely making thousands of IUs of vitamin D daily. Maasai herders have blood levels of 25(OH)D of approximately 40-50 ng/mL. To achieve this level an adult would need to ingest at least 2000 IUs of vitamin D daily; and if obese would require 5000 IUs daily. These are the doses of vitamin D that can sustain a blood level of 25(OH)D of at least 30 ng/ml which is thought to be required for the many of the non-musculoskeletal health benefits of vitamin D. This Narrative Review [Allan, 2016] did not consider the scientific literature on the biological functions of vitamin D and only focused on meta-analyses of studies that used suboptimal doses of vitamin D that either did not measure nor achieve a blood level of 25(OH)D of at least 30 ng/ml. Thus it
provides little insight into the non-musculoskeletal health benefits of vitamin D.”
Dr. Michael F. Holick, PhD, MD
Professor of Medicine, Physiology and Biophysics; Director of the General Clinical Research Center; Director of the Vitamin D, Skin and Bone Research Laboratory;
Director, Biologic Effects of Light Research Center
Boston University Medical Center
Now what?
Most likely, trials with negative findings will have more than one of these tells. Knowing these tells will help you understand possible reasons why the research did not show promising results. On our documentation page we have links to charts and studies which you may find pertinent and helpful to share with family and friends.
Sources
For further details on evaluating vitamin D studies we recommend you refer to the following:
Guidelines for optimizing design and analysis of clinical studies of nutrient effects
Robert P. Heaney, MD
Creighton University
December 2013
Design Components of Interventions/Studies of Vitamin D
Robert P. Heaney, MD
Creighton University
Bruce W. Hollis, PhD
Medical University of South Carolina
December 2014
Studies and Responses
JAMA reports prenatal vitamin D has no effect on early childhood asthma reduction
The Vitamin D Antenatal Asthma Reduction Trial (VDAART) tried to determine whether prenatal vitamin D supplementation could prevent asthma or recurrent wheeze in early childhood. Unfortunately, due to non-compliance by many of the participants, and no on-going vitamin D supplementation after birth – it recorded only small results – a 6% reduction.
Study on Falls in the Elderly
A paper from Bischoff-Ferrari, et al., published January 4, 2016, studied 200 home-dwelling men and women, over the age of 70, in Zurich, Switzerland. The purpose of the study was to assess whether vitamin D would prevent functional decline in the elderly. Reports of falls were also analyzed. The participants were divided into three groups which received monthly doses of vitamin D: 24,000 IU; 60,000 IU; or 24,000 IU of vitamin D3 plus 300 μg of calcifediol (25-Hydroxy vitamin D3).
Study shows increased mortality with high vitamin D levels
A study published February 17, 2015 by Durup et al. reported “A reverse J-shaped association between serum 25-hydroxyvitamin D and cardiovascular disease mortality – the CopD-study.” This backwards J-shape implies that the lowest risk of mortality is in the middle range of vitamin D (70 nmol/L or 28 ng/ml) with an increased risk at low levels (12.5 nmol/L or 5 ng/ml) and a slight increased risk at high levels (125 nmol/L or 50 ng/ml).
Vitamin D Research and Clinical Practice At a Crossroads
Controversy regarding primary care physicians routinely screening for 25(OH)D and prescribing high-dose supplements in the absence of a clear clinical indication may reduce differences in intakes between study groups, jeopardizing the opportunity for the trials to yield informative results.
The IOM got it wrong!
Quite simply, the IOM got it wrong. We have posted comments and information since the Institute of Medicine (IOM) said that the new Recommended Dietary Allowance (RDA) of 600 IU/day was adequate to achieve their recommended level of 20 ng/ml. Our focus has always been that 20 ng/ml was not sufficient. It turns out that there’s an even more serious problem: a review of their statistical methods shows that they were not correct – 600 IU/day will not get 97.5% of the population to 20 ng/ml. Instead it will only get 50% of the population to that level.

