Published on October 26, 2021
Implementing vitamin D screening and targeting a level of at least 40-60 ng/ml (100-150 nmol/L) projected to far outweigh benefits of early detection
Key Points
- According to a study published in 2015, among 1,000 women who start screening at age 50 and are screened for 20 years, 2 to 3 will avoid dying from breast cancer and 200 women will have at least one false positive test, 30 will undergo a biopsy, 3 will be diagnosed with an interval cancer, and breast cancer will be over-diagnosed in 15
- The rough estimate of the financial impact of excess testing and overtreatment following a false positive is close to 4.1 billion dollars each year
- Getting everyone’s vitamin D level up to at least 40-60 ng/ml, assuming an 80% reduced risk of incidence, is a safe and cost-effective intervention that could result in around 225,000 people who would be saved the trauma of breast cancer this year – both the disease itself and the horrific treatment
As October nears an end, so does the month of pink extravaganza promoting Breast Cancer Awareness. The idea is well-meaning, but since its inception in 1985, it has not been able to significantly affect change in the incidence of breast cancer.
According to the Maurer Foundation, breast cancer rates for women under 50 years of age have remained stable since 1985, and breast cancer rates for women over 50 have remained stable since 2003. In terms of mortality, African American women have worse statistics, with breast cancer mortality rates 41% higher than the mortality rate of non-Hispanic whites by the year 2007.
During these 14-36 years, we have continued to pink-ify October and increase breast cancer awareness, and yet it seems to have had zero to little impact on what to do to effectively prevent or reduce breast cancer.

Does Early Detection Save Lives?
The statistic that 1 in 8 women will be diagnosed with breast cancer in their lifetime has remained stable, even with breast cancer awareness taking over our health care system. Today, the US Preventive Services Task Force recommends a mammogram every two years for women 50-74 years of age. This translates into 13 mammograms for every woman, most often with no symptoms, no preexisting breast cancer, no previous diagnosis of breast lesion, no known genetic mutation (such as BRCA1 or BRCA2), and no history of chest radiation at a young age.
Is it working? Is this the best course of action to prevent breast cancer, and to prolong lives?
Is it worth it?
Is it worth a false-positive or an unnecessary biopsy? The paper, Benefits and harms of mammography screening, by Loberg et al. concludes
“Women should be correctly informed about the benefits and harms of mammography screening (Figures 1 and 2). A comprehensible way of communicating information on benefits and harms of mammography screening is presented in Figure 1: among 1,000 women who start screening at age 50 and are screened for 20 years, 2 to 3 will avoid dying from breast cancer and 200 women will have at least one false positive test, 30 will undergo a biopsy, 3 will be diagnosed with an interval cancer, and breast cancer will be overdiagnosed in 15.”
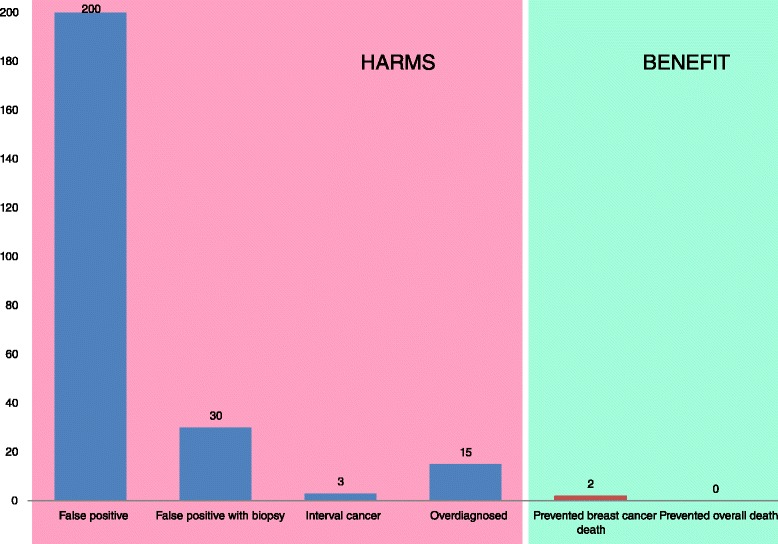
Figure 1, Loberg et al., Breast Cancer Research (2015)
False positive – an identification of a breast tumor, when there is none. Data cited by Loberg indicate that over a 10 year period 30% of women in the US will have a false positive result, and 50% will experience a false positive in their lifetime! He also states that it takes up to 2 years for those false positives to be cleared and that women experience three years of psychological harm after screening.
False positive with biopsy –Women who undergo a biopsy, unnecessarily, due to a false positive.
Interval cancer – Cancers detected between mammogram screenings, that could have been overlooked or are rapidly growing tumors.
Overdiagnosis – In this case, the cancer is there, but is not relevant. This can apply to both in situ and invasive cancers. In other words, by the time the woman dies cancer would not have progressed to any stage that would have caused her health problems. So, while the cancer is actually there – the diagnosis causes stress during the remaining lifetime and doesn’t lead to a longer or more fulfilling life, and/or the treatment may lead to illness or death.
Figure 2 from Loberg’s paper (below) most adequately explains over-diagnosis and identifies four different possibilities, none of which prolongs life.
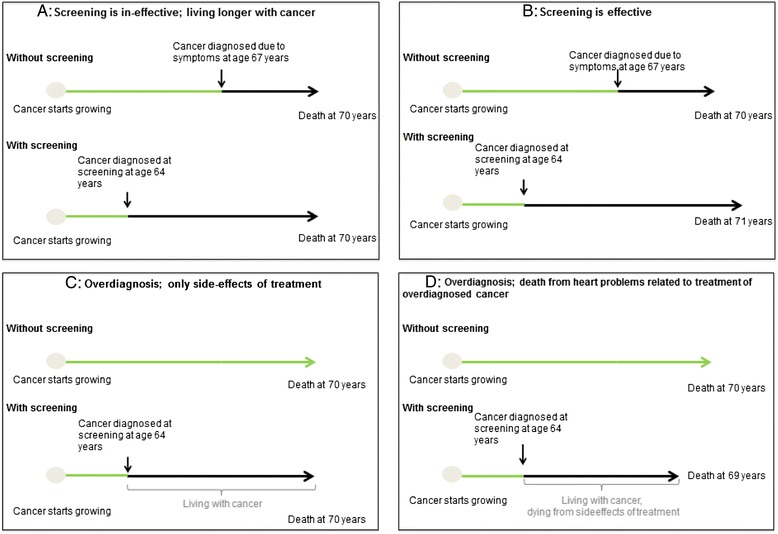 Figure 2, Loberg et al., Breast Cancer Research (2015)
Figure 2, Loberg et al., Breast Cancer Research (2015)
Do mammograms prevent death?
Loberg gets to the meat of the issue with the final figure of the paper:
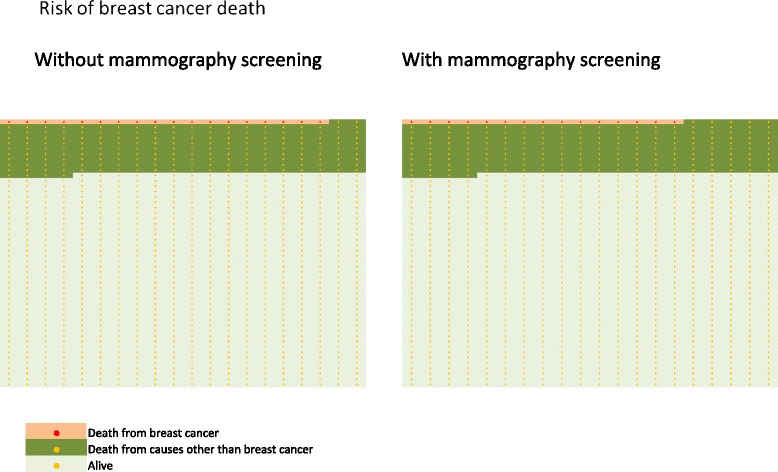
Figure 6, Loberg et al., Breast Cancer Research (2015)
If you examine where the dark green area (all death) meets the pale green area (alive) – it is in the same place. The only difference, Loberg concludes, is whether you died of breast cancer or other causes (as you see there is more light pink area along the top of the graph in the non-mammography chart).
What is the financial impact of all this testing and overtreatment?
In Cost of Breast-Related Care in the Year Following False Positive Screening Mammograms by Chubak et al. (2010), they estimate an additional $503 in health care costs for the year following a false positive. That might not sound like much, but let’s do a quick and dirty analysis for the US…
| 308 million | population of US in 2010 |
| 156,464,000 | Women in the US (50.8 % – source: Women’s Health USA) |
| 54,136,544 | Women 50 or older – (34.6 % source: Women’s Health USA) |
| 27,068,272 | # Mammograms in the US a year. Assume every woman over 50 is following the suggested guideline of a mammogram every two years. |
| 8,120,482 | False positives per year. (Loberg et al. – 30% false positives) |
| $ 4,084,602,245 | Cost per year of false positives. (Chubak et al. – $503 additional cost for a false positive) |
A very rough estimate of… $ 4.1 BILLION!
How do we truly affect change in breast cancer?
Vitamin D has been associated with between 50-80% reduced risk of breast cancer incidence, depending on the study. GrassrootsHealth recommends getting your vitamin D level tested and maintaining a level of at least 40-60 ng/ml (100-150 nmol/L) to help prevent many diseases, including cancer.
According to breastcancer.org, an estimated 281,550 new cases of invasive breast cancer and 49,290 cases of non-invasive breast cancer are expected to be diagnosed in the United States in the year 2021. What if everyone started now with getting their vitamin D levels up? Assuming an 80% reduced risk of incidence that would be around 225,000 people who would be saved the trauma of breast cancer this year – both the disease itself and the horrific treatment.
Would it be worth implementing a new standard of care, which tests vitamin D levels twice a year until each person got their level over 40 ng/ml (100 nmol/L) and then once a year thereafter? GrassrootsHealth and 48 scientists say, “Yes!”
Join us today!
- Get your vitamin D level checked and maintain 40-60 ng/ml (100-150 nmol/L).
- Tell your friends, like our facebook page and share our information.
- Donate to GrassrootsHealth – as we enroll 1,000 more women in our Breast Cancer Prevention project.
Keeping Up with Your Vitamin D is an Essential Part of Staying Healthy
 Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health now and for your future. Choose which to measure, such as your vitamin D, omega-3s, and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. You can also track your own intakes, symptoms and results to see what works best for YOU.
Having and maintaining healthy vitamin D levels and other nutrient levels can help improve your health now and for your future. Choose which to measure, such as your vitamin D, omega-3s, and essential minerals including magnesium and zinc, by creating your custom home test kit today. Take steps to improve the status of each of these measurements to benefit your overall health. You can also track your own intakes, symptoms and results to see what works best for YOU.
Enroll and test your levels today, learn what steps to take to improve your status of vitamin D (see below) and other nutrients and blood markers, and take action! By enrolling in the GrassrootsHealth projects, you are not only contributing valuable information to everyone, you are also gaining knowledge about how you could improve your own health through measuring and tracking your nutrient status, and educating yourself on how to improve it.
References
Benefits and harms of mammography screening
Magnus Loberg et al.
Breast Cancer Research
May 2015
Read Paper
Cost of Breast-Related Care in the Year Following False Positive Screening Mammograms
Chubak et al.
Medical Care
September 2010
Read Paper
An Open Letter to the New York Times
Cedric Garland
December 2009
Read Letter (scroll down page)
The Problem with National Breast Cancer Awareness Month
Women’s Health
Robin Hilmantel
October 2015
Read Article
The Big Squeeze
A Social and Political History of the Controversial Mammogram
Handel Reynolds, MD
Cornell University Press
2012
Read Part of Book





